Key Takeaways
Discover the top diabetes innovations of 2026 and how you can harness digital tools, next-gen medications, and smarter care models for easier, healthier daily living. Here’s what you need to know to personalize your diabetes plan and make the most of today’s groundbreaking strategies—without information overload.
- CGM and automated insulin delivery are now standard for most people with diabetes, giving you real-time data and fewer fingersticks from the moment of diagnosis.
- AI-powered apps and decision support tools cut down on daily guesswork, offering personalized dosing advice and automated reminders right from your phone.
- GLP-1 and dual GIP/GLP-1 medications deliver more than sugar control, driving 8–12% weight loss and extra heart, kidney, and liver protection—all with fewer injections.
- Lifestyle tweaks are more powerful than any fad diet: aim for 150+ minutes of movement and 5–7% weight loss to see major gains in blood sugar and heart health.
- Modern care is a team sport: expect collaborative planning with educators, pharmacists, and community health workers, plus digital coaching for daily support.
- Special population focus: older adults get safer, easier routines with smarter CGMs; kids and teens benefit from family-centered tech and school support; and hospitals now use your devices for seamless transitions.
- Emerging research means more freedom: AI coaches, wearable nerve-stimulation devices, and expanding medication options are pushing diabetes care toward less hassle and more customization.
- Personalization is key in 2026: combine cutting-edge tech, user-friendly meds, and real-world support to build a diabetes plan that fits your unique goals and lifestyle.
Ready to upgrade your diabetes care? Dive into the full article for expert tips, innovative tools, and actionable steps to transform your daily life.
Introduction
Ever wished your phone could spot a dangerous blood sugar swing before you feel it—or even suggest the right dinner tweak for steadier numbers? In 2026, that’s just everyday reality for tens of millions managing diabetes.
Forget the old routine of endless fingersticks, food math, and crossed fingers. New tech—like continuous glucose monitors, AI-powered coaching, and automated insulin pumps—now forms the backbone of modern diabetes care, making life smoother for everyone from executives to busy parents.
What’s different right now? Three things drive this transformation:
- Real-time insights: Devices and apps now translate complex CGM data into easy actions you’ll actually use.
- Personalized, smarter medications: Once-weekly GLP-1 injectables and pills don’t just lower blood sugar—they protect your heart, kidneys, and waistline.
- Integrated team support: Digital self-management and connected care teams mean you adjust fast, not weeks behind the curve.
Recent guidelines are clear: these breakthroughs aren’t just for “techies” or early adopters—they’re reshaping standards for anyone living with diabetes or at risk. The result? More freedom, less stress, and solutions that fit your life instead of the other way around.
As a tech-interested professional, you’re probably asking: Which tools are actually worth your time? How do you tailor this new wave of innovation to your real-world needs, priorities, and workflows?
In this guide, you’ll get a clear window into:
- The newest technologies changing daily diabetes life
- AI-driven decision support and digital coaching
- Game-changing medication strategies and how to personalize them
- Evidence-backed nutrition, movement, and lifestyle tools
- The mind-body connections and team models that support sustainable results
Ready to see how diabetes care in 2026 puts innovation (and control) back in your hands? The landscape is changing fast—let’s set you up to make the smartest next move.
First up: discover which technology upgrades are already revolutionizing daily routines—no doctorate required.
The Technology Transformation: 2026 Tools Changing Daily Diabetes Life
The New Normal: CGM, Smart Pumps, and Automated Insulin Delivery
Picture this: instead of juggling fingersticks and math just to eat breakfast, you check your phone and instantly know if it’s a good morning for pancakes. That’s the power of continuous glucose monitoring (CGM)—and in 2026, CGM is now recommended from diagnosis for all ages, not just for “advanced” users.
Updated standards state CGM should be offered to:
- Anyone with type 1 diabetes
- People with type 2 on insulin
- Those at risk for lows—even without insulin
- Anyone who benefits from extra feedback
Automated insulin delivery (AID)—including hybrid closed-loop systems and the iLet Bionic Pancreas—has moved from “specialist tech” to a recommended standard for most people using insulin. These systems:
- Adjust insulin automatically, around the clock
- Cut down manual calculations and reduce fingersticks
- Boost time in range and streamline life
- Offer new features focused on user experience, like real-time meal detection
You’ll see these innovations transforming daily routines, especially as coverage barriers shrink and interfaces get friendlier. “Spend less time treating diabetes, more time living your life”—that’s a shift worth sharing.
AI Decision Support & Digital Self-Management: Real-World Impact
What if your diabetes care felt smarter—not just “easier”? In 2026, AI-powered tools are taking center stage. The latest guidance calls for widespread use of:
- Digital self-management apps with automated reminders
- AI decision-support systems (like PCM-DSS) that read your CGM + med data and suggest tailored dose changes
- AI-driven retinal screening—allowing earlier, broader access to crucial eye care
Clinicians now use these systems to optimize complex medication regimens faster. You'll notice less guesswork, fewer “data overload” moments, and more targeted adjustments. Imagine your phone pinging: “Great average this week! Want to tweak dinner carbs for even steadier results?”
“The future of diabetes care is connected, predictive, and increasingly automatic.” That’s a screenshot-worthy quote.
How These Innovations Change Life With Diabetes
Life with diabetes in 2026 looks lighter: less stress about numbers, fewer alarms, and more freedom to focus on work, family, and fun.
Here’s what you can expect from a fully integrated tech approach:
- Fewer fingersticks, more stable readings
- Less “diabetes brain space,” giving you emotional breathing room
- Faster problem-solving with your care team—show them your latest CGM+AI trends, and you’re brainstorming together, not just reporting numbers
When considering new tools, ask your team about coverage, compatibility with your lifestyle, and whether you’ll benefit from digital coaching or extra in-person support.
The most actionable move: if you haven’t discussed CGM, advanced pumps, or AI apps with your provider recently, 2026 is the year to start. In this new era, technology isn’t just an upgrade—it's the foundation for a better, more livable daily diabetes experience.
Breakthrough Medication Strategies: 2026’s Most Powerful Approaches
GLP-1, Dual GIP/GLP-1, and the SGLT2 Era
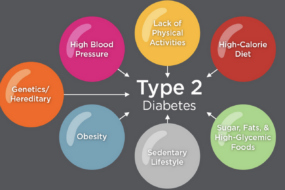
The 2026 diabetes playbook starts with GLP-1 receptor agonists and dual GIP/GLP-1 agents—medications that do more than just lower blood sugar.
These drugs:
- Promote significant weight loss (often 8–12%+)
- Lower A1C and improve cardiovascular, liver, and kidney outcomes
- Are now recommended for adults with type 2 diabetes who also have obesity, heart failure, chronic kidney disease, or liver issues
Picture this: Once-weekly injections or a pill, lighter day-to-day management, and protected hearts and kidneys.
Physicians are updating treatment algorithms to put cardio-renal-hepatic safety at the top, not just glucose targets.
“These meds turn daily treatment into long-term protection—2026 makes it clear: good diabetes care means better health everywhere, not just a lower A1C.”
Personalizing Noninsulin Therapy and Complex Cases
Choosing the right noninsulin therapy now means matching medications to your unique mix of age, comorbidities, and risk of lows—not just picking by numbers.
2026 guidelines recommend:
- Favoring drugs with low hypoglycemia risk for older adults, and anyone at high risk for falls
- Integrating obesity pharmacotherapy with careful dose titration to maximize results without tough side effects
Think of your pharmacy shelf as a custom toolkit—each med fits a specific need, from blood pressure to weight loss and even smoother transitions through life stages.
“Smart prescribing is about the right fit for your story—one size never fits all in 2026.”
Special Medication Situations: Oncology, Steroids, and Transplant
Modern diabetes care takes treatments beyond the basics.
Here's how the latest standards tackle tricky scenarios:
- With cancer therapies (PI3K, mTOR inhibitors): Use metformin unless severe hyperglycemia demands insulin, since insulin may interfere with cancer meds
- For steroid-induced highs: Adjust medications proactively—don’t wait for blood sugars to surge
- Post-transplant: Layer in GLP-1s when possible; tailor insulin carefully
Real-world? Picture a hospital team that tweaks meds for every twist, minimizing double-risk from new illnesses and treatments.
Medication Advances and Quality of Life
2026’s biggest win is making life with diabetes lighter.
- Fewer hospital trips
- More once-weekly injections
- Fewer daily alarms and less worry
Watch for:
- New non-injectable formulations under development
- Side effects such as GI upset or rare hypoglycemia—always discuss pros and cons with your clinician
“In 2026, diabetes feels less like a full-time job and more like a background app—always working, rarely interrupting.”
Today's diabetes meds offer so much more than “sugar control”—they boost heart, kidney, and even mental health, all in one plan. The best move? Talk with your team about the latest options, and personalize your medication lineup for better living—not just better numbers.
Lifestyle, Nutrition & Weight: The Core of Modern Diabetes Prevention and Control
2026’s Foundations: Evidence-Based Goals for Real Change
Picture this: You’re not counting every carb but walking into a room with energy and confidence, knowing your numbers are in range most days.
For diabetes prevention, the new baseline is clear:
- ≥7% weight loss for those at high risk
- 150+ minutes of moderate activity per week—think brisk walks, easy cycling, or long dance sessions
- Coaching models that mix digital check-ins and in-person support, so you’re never flying solo
If you already have diabetes, aim for 5–7% weight reduction—this level significantly improves blood sugar and heart health, even if you’re nowhere near “ideal” body weight.
Integrating nutrition, behavioral support, and real-world strategies beats any “all-or-nothing” plan. Success comes from small, sustainable shifts.
“Sustainable lifestyle tweaks beat ultra-restrictive diets every time—think long-game, not quick fix.”
Strategic Overview: 7 Nutrition Secrets Backed by Science
The top 2026 research says flexibility beats rigidity, so forget one-size-fits-all. Here’s what gets results:
- Mediterranean style eating—bring on colorful veggies, fish, olive oil, and legumes
- Smart low-carb—cutting starches and sugars without banning all carbs
- Intermittent fasting—works for some, especially those who like structure
- Meal planning tailored to your culture and preferences, not someone else's template
- Focus on these food groups:
- Nonstarchy veggies and whole fruits
- Lean proteins
- Whole grains, nuts, and seeds
- Legumes and low-fat dairy
- Minimize:
- Sugary drinks, sweets, red meats
- Refined grains and ultra-processed foods
- Supplements rarely work for diabetes control—current advice is, spend your money on quality food
“What you put on your plate matters more than chasing the latest diet trend.”
Exercise: The Diabetes Outcomes Multiplier
Movement isn’t negotiable—it’s core therapy. The magic number for adults is:
- 150+ minutes of moderate activity weekly, plus strength sessions
- For youth: at least 60 minutes a day, mixing aerobic and bone-building moves
Mix it up:
- Strength training—preserves muscle, boosts metabolism
- Aerobic activity—reduces fatigue, steadies blood sugar
- Lifestyle movement (think: walking meetings, daily chores)—every step counts
Smart 2026 tips:
- Prevent lows and highs by using CGMs paired with exercise alerts
- New routines combine fitness with fun, like streaming workout videos or virtual group classes
“Move your way—how you move is less important than getting moving.”
Small shifts in meals, movement, and mindset—built on real science—are your core levers for diabetes prevention and control in 2026. Start with what fits your real life, and you’ll see the benefits compound day by day.
The Future of Person-Centered, Psychosocial, and Team-Based Diabetes Care
Building Your Team: Collaborative, Individualized Care Models
Picture this: your diabetes care feels less like doctor’s orders and more like a collaborative project with people who get your life.
2026 standards put you at the center—expect shared decision-making where your work, culture, and daily realities matter as much as your numbers.
Your care team goes beyond your doctor:
- Community health workers help manage risk factors and get resources right where you are.
- Expert pharmacists guide medication adjustments, answer questions, and clarify side effects.
- Certified diabetes educators break down complex regimens and support real-world change.
Quote: “The best diabetes plan is one that fits your real life, not just your A1C.”
Diabetes Self-Management Education & Support (DSMES): Maximizing Engagement
DSMES isn’t one-and-done; it’s a toolkit you refresh at every big moment:
- At first diagnosis—because everything’s new.
- Annually—or when sticking to goals becomes tough.
- During treatment changes, complications, or major life transitions.
To make it stick, DSMES now prioritizes:
- Tailoring programs to your culture, language, and learning style.
- Digital tools—think interactive apps and smart reminders to keep you moving forward.
- Behavioral techniques that focus on habits for real-world success.
Want confidence advocating for yourself at appointments? This is where you build those skills. “Empowering you means more than instructions—it's about building lasting confidence.”
Addressing Emotional Well-being & Social Determinants
True diabetes care now checks on your head and heart, not just your blood sugar.
- Routine screenings for well-being and diabetes distress catch silent struggles early—60% of people report emotional burnout at some point.
- New behavioral health models blend resilience training with medical visits.
- Employers are encouraged to adjust policies for diabetes tech use at work, making daily management smoother.
To make care fit your reality:
- Providers now adapt plans to your resources, insurance, schedule, and housing situation.
- Expanded access to support services narrows gaps caused by location or income.
Quote: “It’s no longer just about doctors and meds—it’s about a system designed to work for you, wherever you are.”
These trends mean you get a tailored, practical plan that values life outside the clinic—delivering support, flexibility, and fresh tools when you need them most.
Special Populations & Unique Care Considerations
Older Adults: Staying Safe, Independent, and Energized
Picture this: You’re 70 and want true independence. Continuous glucose monitoring (CGM) is now recommended for every older adult using insulin, making fewer fingersticks and dangerous lows possible—even for those with memory or vision challenges.
Key 2026 updates focus on:
- Hypoglycemia avoidance tools—smarter CGMs now send out-of-range alerts to caregivers and care teams instantly
- Protein intake at ≥0.8g/kg/day to preserve muscle, especially during weight loss or illness
- Personalized exercise plans to minimize falls and fractures, with workouts adapted for varying mobility
When it comes to meds, updated algorithms recommend:
- Choosing drugs with very low hypoglycemia risk (think DPP-4s, SGLT2s, or GLP-1s)
- Setting glycemic targets that protect cognition and bone health—even if A1C isn’t ultra-low
“The right diabetes tech and tweaks can keep you stronger, steadier, and safer—without endless monitoring.”
Children, Adolescents & Family Empowerment
Managing diabetes for kids is a team sport in 2026. Family-centered care is the foundation, empowering both parents and young people with real-time tech and community connections.
Today’s must-haves include:
- Caregiver and school staff training—so everyone from teachers to coaches can help spot and address lows
- Flexible lunch and snack guidance that fits busy schedules and picky eaters
- Modern CGMs and, in some cases, age-appropriate GLP-1 or SGLT2 therapy
- Coaching for smooth self-care transitions as kids head to college or work
Imagine a seventh grader confidently scanning their CGM at school—supported by a team, not alone.
“Family support—and the right tech—can turn diabetes from a burden into a skill set for life.”
Diabetes Care in the Hospital and Beyond
Hospital stays just got less stressful thanks to expanded diabetes technology protocols in 2026. Your hospital may now use your own CGM or insulin pump, reducing errors and fingersticks.
Rapid changes include:
- Up-to-date perioperative protocols for insulin and GLP-1s to minimize swings during surgery or acute illness
- Discharge planning that actually works—teaming with your home provider to update devices and scripts before you walk out the door
- Standardized data sharing between inpatient and outpatient teams, smoothing every transition
Visualize a care handoff where your time-in-range stats go straight from hospital staff to your home clinic—no lost charts, no confusion.
“Seamless transitions and better-connected teams mean you recover safely and get back to living, faster.”
Across all ages and settings, 2026 diabetes care is about tailored tools, smarter teams, and making sure your needs drive every recommendation, not just your numbers.
On the Horizon: Emerging Research and Future Possibilities
The Rise of Smart AI Care: TREAT2D and Beyond
Imagine AI that not only tracks your data but suggests your next best diabetes move—automatically. That’s exactly what trials like TREAT2D are testing in 2026, where AI-powered decision support crunches CGM, medication, and lab data to recommend real-time tweaks to complex regimens.
- In recent pilot studies, systems like PCM-DSS have reduced manual medication adjustments by over 40%.
- According to fresh ADA guidance, AI is now encouraged for virtual coaching, medication titration, and automated risk alerts—especially as more people manage diabetes remotely or outside traditional clinics.
- The next-gen vision: remote, virtual-first diabetes care that minimizes office visits and maximizes proactive support.
“AI is becoming the coach in your pocket, eliminating trial-and-error for thousands.” Picture this: your app flags a trend, nudges your provider, and suggests a fix—no waiting weeks between appointments.
New Therapies: Devices, Neuromodulation & Drug-Free Breakthroughs
Move over, medications—2026 sees a surge in neuromodulation and non-drug tools. Early trials are tapping into the body’s own nerve signals to improve glucose patterns without drugs.
- Current research is focused on candidates with type 2 diabetes not responding to standard meds.
- Devices gently stimulate the vagus or other nerves, aiming for real improvements in insulin sensitivity and daily blood sugars.
- “Future diabetes care could look more like physical therapy—with wearable tech* than a medicine cabinet.”
Envision a future where you swap a daily pill for a 20-minute wearable session. Early signs point to fewer side effects and improved adherence—though experts note costs and long-term impact still need study.
Expanding Drug Indications: Vascular Protection for All
The GLP-1 revolution isn’t slowing. Now, studies are drilling into how GLP-1 and dual GIP/GLP-1 agonists might protect blood vessels and prevent hypoglycemia—even in type 1 diabetes, not just type 2.
- Ongoing clinical trials are evaluating outcomes like fewer heart attacks, strokes, and severe lows in new groups.
- Early results show promise for expanding these therapies to younger ages and unique comorbidities.
It’s a “watch-this-space” moment—these drugs are moving from controlling sugar to potentially rewriting the rulebook for heart, kidney, and neuroprotection.
Groundbreaking research is setting the stage for AI-augmented care, drug-free devices, and broader medication benefits—all aiming for more responsive, less burdensome diabetes management. The future looks smarter, more connected, and packed with options you and your care team can tailor—not just someday, but starting now.
Tailoring Strategies: Personalizing Your 2026 Diabetes Plan
Start With Your Big Goals—and Key Factors
Personalizing diabetes care in 2026 means zeroing in on your main outcomes, your diabetes type, and your everyday realities.
Whether your priority is weight loss, fewer lows, fewer injections, or lasting heart/kidney protection, start by listing your top goals—then filter new advances through that lens.
Picture this: you want more energy and less fingerstick hassle. With CGM now recommended from diagnosis for nearly anyone, you might immediately qualify for a device that provides 24/7 glucose data and alarms.
Personalization in Practice—Ask These
To get a plan that’s truly custom-fit, discuss these points with your care team:
- Your diabetes type, age group, and medication history
- Any priorities (weight, sleep, sports, work travel, pregnancy)
- Past side effects or barriers with meds/devices
- Financial/insurance coverage or tech access
- Desired phasing (“How fast can I start this?”)
Want practical fuel for this conversation? Here are a few quotable prompts to take into your next appointment:
- “If you were aiming for fewer daily decisions, what tech from 2026 would you recommend for me?”
- “For someone with priorities like mine, where do GLP-1-based meds or AI tools fit?”
- “Can we design a plan that focuses on prevention—even if my A1C is stable?”
“One Size Fits None”: Real-World Combinations
2026 is all about synergy—combining the strengths of new medications, AI-powered adjustments, and team guidance.
A few combos to inspire you:
- Pair once-weekly GLP-1/dual agonists with a lifestyle plan (for weight loss, heart-kidney gains, or convenience)
- Stack CGM and automated pumps if your main outcome is smooth glucose with less daily math
- Tap digital coaching or DSMES when big life changes or stress threaten your routines
“Modern diabetes care is like building your ultimate toolkit, not settling for a prefab approach.” Picture a daily routine where your phone, watch, and care team all “get you”—from food preferences to travel needs.
This approach puts power in your hands: choose the pieces that create the easiest, safest, and most rewarding life possible. If you want less daily hassle, greater health protection, or a plan that fits your real routine, personalizing your diabetes strategy in 2026 turns those wishes into a doable action plan.
Conclusion
Stepping into 2026, diabetes care is no longer about just “keeping up”—it's about leaning in to innovations that let you live lighter, healthier, and on your own terms.
You now have an expanding toolkit of smart technologies, powerful meds, and personalized support to transform daily care from a constant grind into a more seamless, empowering experience. The real win? More freedom, less stress, and greater control—all grounded in science and tailored for your unique life.
Here’s how to turn new strategies into better living right now:
- Schedule a deep-dive conversation with your care team about emerging options like CGMs, advanced medications, and AI apps—align tech with your lifestyle, not the other way around.
- Revisit your top diabetes goals (energy, weight, fewer lows, heart protection) and filter new advances through what's most important for you.
- Explore digital coaching or DSMES refreshers to build skills, confidence, and community support when facing life changes or plateaus.
- Start small with sustainable shifts—a new walking routine, upgraded meal planning, or trialing an app—compound impact always beats quick fixes.
- Advocate for care that honors your real life—bring up work, travel, or emotional needs at every visit so your plan actually fits.
Ready to take charge of your diabetes journey?
- Book that appointment and hold nothing back—bring your priorities, barriers, and “wish list” to the table.
- Download a recommended self-management app and set your first goal today.
- Connect with others—whether it’s a support group, digital forum, or family meeting, momentum grows faster together.
2026 puts the steering wheel in your hands: smarter tools, stronger teams, and real choices add up to a life with diabetes that’s lighter, brighter, and truly yours.
This is your moment to act. Embrace the breakthroughs—your best years with diabetes start now.