Key Takeaways
When navigating menopausal joint pain, understanding the link between hormones and your aches is a game-changer. Here’s what matters most if you’re considering hormone therapy, with actionable tips you can use or discuss with your provider today.
- Estrogen decline during menopause triggers joint pain by increasing inflammation and reducing natural lubrication, making stiffness especially common in the hands, knees, hips, neck, and back.
- Hormone therapy (HRT) delivers proven but modest relief for menopausal joint pain, showing about a 5–10% drop in pain scores over two years in research studies—think “turning down the volume,” not silencing it.
- Best results occur when HRT starts within 10 years of menopause onset and targets those with new, widespread joint aches combined with classic menopause symptoms like hot flashes or sleep disruption.
- HRT fits best as part of a bigger plan—for real gains, combine therapy with exercise, anti-inflammatory foods, and regular symptom tracking to maximize comfort and mobility.
- Risks and benefits of HRT vary: While most healthy women see mild improvements, there’s a minor increase in risks like blood clots and stroke—so joint pain relief should always be weighed against your medical history.
- Not every joint pain is menopausal: If symptoms appeared long before menopause, are severe, or come with major swelling or heat, work with your clinician to rule out other causes before starting HRT.
- Transdermal patches and ultra-low-dose HRT lead current innovations by offering customized, lower-risk approaches—talk with your provider about the latest options that might suit your lifestyle.
- Personalized, evidence-based decisions are essential: Matching the timing, type, and dose of HRT to your unique joint pain pattern ensures you get the most from therapy—smart selection means better results.
Ready to move from confusion to confidence on hormone therapy for joint pain? Dive into the full article for expert-backed answers and real-life strategies to keep you moving smoothly through menopause.
Introduction
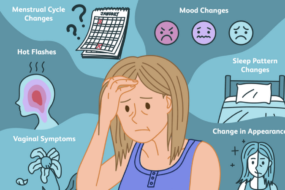
Wake up feeling like your joints aged overnight—stiff fingers, sore knees, hips that creak? Nearly half of menopausal women know that sensation all too well, yet it’s a symptom that often slips under the radar.
That ache isn’t just in your head—or your running shoes. Hormonal shifts during menopause can trigger real, persistent joint pain, sometimes showing up before the classic hot flashes or night sweats. If you’ve ever wondered why sudden aches set in as soon as your cycles went sideways, you’re not alone.
Here’s the good news: The confusing world of menopause and joint pain isn’t a mystery reserved for medical journals. Recent research has revealed that hormone therapy (HRT), when carefully considered, may offer relief that science can back up. But it’s not a magic fix—and the real picture is far more nuanced than the headlines suggest.
You’ll find out:
- How hormone drops actually impact your joints (think: estrogen as your body’s joint “oil”)
- When joint pain is most likely connected to menopause—and when it’s not
- What the evidence really says about hormone therapy for aching, stiff joints
- The trade-offs, candid risks, and questions you’ll want to review before making any decisions
- How to tailor a real-world plan—integrating everything from AI-powered symptom trackers to anti-inflammatory hacks
You’re tech-savvy, data-driven, and used to optimizing your workflow—why not apply that same logic to your own health decisions? Whether you’ve been wrestling with morning stiffness or puzzling over whether HRT is worth the buzz, this guide will help you separate hype from actionable solutions.
Ready for an honest look at why your knees (and hands, and hips) are acting out—and what hormone therapy might actually bring to the table? Let’s unravel how menopause and joint pain truly connect, starting with a clear view of what’s happening inside your body.
The Connection Between Menopause, Hormone Changes, and Joint Pain
When menopause hits, your hormone levels—especially estrogen—drop dramatically.
This decline sets off a chain reaction in your entire body, but your joints notice the difference first. Many women describe it as “suddenly waking up with stiff, aching knees or hands.”
Why Estrogen Matters for Joint Health
Think of estrogen as the oil in your car engine: it keeps everything moving smoothly, from cartilage to fluid inside your joints.
As your estrogen drops:
- Inflammation rises, making your joints feel puffy or sore
- Cartilage protection weakens, so “creaky” sensations and more wear-and-tear can develop
- Synovial fluid production dips, which means less natural joint lubrication
- Your brain’s pain sensitivity switches up, leading to aches and stiffness that feel new or worse
Classic Menopausal Joint Pain Patterns
Wondering if your pain is menopause-related? Picture this common pattern:
- Achy, stiff joints—often in the hands, knees, hips, neck, or back
- Morning stiffness that usually eases after you get moving
- “Traveling” joint pain, where discomfort appears in new areas every few weeks
- Mild swelling or puffiness without redness or major heat
For about 50% of women, joint pain and stiffness become noticeably worse during perimenopause and the first years after menopause. That’s not rare—it’s one of the most common symptoms, though often overlooked.
Not All Joint Pain Means Menopause
Here’s a quick checklist to help you tell the difference:
- Menopause-related joint pain: New, generalized pain coinciding with other menopausal changes (think hot flashes, sleep issues)
- Osteoarthritis: Gradual, progressive wear in one or two major joints, usually older adults
- Autoimmune disease (like rheumatoid arthritis): Persistent, severe swelling and pain, often with redness and heat
- Injury or overuse: Clear connection to an event or activity (twisted knee, tennis elbow, etc)
If symptoms started around the same time as your periods changed, it’s a big clue menopause is involved.
Key Takeaways for Fast Action
- New, wide-ranging joint pain around menopause is common and often linked to hormonal changes
- Track your symptoms and patterns—share these details with your provider
- If pain is sudden, severe, or only in one joint, get checked out to rule out other causes
Expect some morning stiffness or aching, but if joint pain disrupts your daily life or comes with unusual swelling, see a clinician. For many women, recognizing this hormone connection is the first step to feeling better—“Just like keeping your car well-oiled, knowing when your ‘joint engine’ needs support can help you stay on track.”
How Hormone Therapy Works for Menopausal Joint Pain
Hormone replacement therapy—also called HRT—is a treatment designed to supplement the body’s declining hormones during menopause, especially estrogen.
HRT comes in two main regimens:
- Estrogen-only (for women without a uterus)
- Combined estrogen and progestogen (for women with a uterus)
Both are available as pills, patches, gels, or sprays, letting you and your clinician personalize the approach.
Estrogen’s Effects on Joints
Picture this: estrogen is like oil for the body’s joint engine—keeping things supple and reducing friction.
Here’s how HRT works to ease joint issues:
- Reduces inflammation in joint tissues, which can mean less pain and stiffness
- Supports cartilage health (the body’s shock absorber)
- Increases joint fluid production, boosting lubrication
- May “dial down” the brain’s pain sensitivity, making everyday aches less intrusive
What the Research Says
You’ll want the science, not wishful thinking.
Let’s look at the numbers:
- The Women’s Health Initiative found a modest but real drop in joint pain for women on estrogen-only HRT (about 5-10% lower pain scores than placebo over two years)
- A Japanese study with perimenopausal women showed measurable improvements in hand pain and function for those using HRT over non-hormonal therapies
- Clinical reviews and meta-analyses note that muscle, bone, and joint benefits of HRT are real, but typically moderate—think of HRT as “dialing down the volume,” not muting it
When HRT is Most Likely to Help
Maximum benefit isn’t guaranteed for everyone. Here’s when HRT is most likely to help:
- Joint pain starts or worsens around menopause transition (vs. long-standing, pre-existing pain)
- You also have hot flashes, sleep trouble, or other menopause symptoms
- Treatment begins within the “window of opportunity”—ideally within 10 years of menopause onset
What Results Should You Expect?
Don’t expect a miracle cure—HRT usually brings partial relief, not a full reset.
A shareable tip: “If menopause turned up your joint pain, HRT might dial it back—but don’t expect complete silence.”
Imagine opening a stubborn jar with less hand pain after three weeks on the right regimen—that’s the kind of win you might see.
For many, the real power of HRT is as one part of a bigger strategy—combining medication, lifestyle tweaks, and clinical guidance.
Key takeaway: Hormone therapy offers proven but modest joint relief for the right candidates—so work with your clinician to see if it fits into your personalized joint pain game plan.
Weighing the Benefits and Risks of Hormone Therapy
Evidence-Based Benefits
If you’re considering hormone therapy (HRT) for menopausal joint pain, here’s what the research actually shows: HRT offers mild to moderate relief for joint aches, stiffness, and swelling triggered by menopause.
Most large studies—including the Women’s Health Initiative—found that estrogen-only therapy reduced joint pain severity by a small yet noticeable margin over 1–3 years.
Beyond pain, HRT provides additional musculoskeletal perks:
- Slows bone loss (reducing osteoporosis risk)
- Helps preserve muscle mass, supporting mobility and strength
- Lowers fracture risk in postmenopausal women
The benefits are most pronounced if:
- Joint pain began or worsened right as menopause symptoms started
- You’re also dealing with hot flashes, sleep problems, or night sweats
- You’re within the “window of opportunity”—less than 10 years postmenopause
“Think of estrogen like WD-40 for your joints—everything moves a bit smoother for many, but it won’t fix dents in the engine.”
Risks, Limitations, and Uncertainties
It’s just as crucial to know what HRT can’t do—and where caution matters. Standard HRT risks still apply, including:
- A slightly increased risk of blood clots (VTE) (about 2–4 cases per 1,000 women over 5 years)
- Small increases in risk of stroke and, for combined regimens, breast cancer and possibly heart disease
- For some, joint swelling may occur, especially with certain estrogen-only formulations
Not everyone sees improvement—up to 40% of women report little or no joint pain relief with HRT.
Evidence supporting HRT for joint pain alone is weaker than for hot flashes or bone loss, meaning it’s best reserved for those with multiple menopausal symptoms.
It’s essential to work closely with your clinician to consider:
- Your age and time since menopause
- Current or past medical issues (such as breast cancer or clotting disorders)
- Personal risk tolerance and lifestyle factors
Real-World Application
Picture this: a healthy woman, eight years into menopause, starts experiencing new knee and hand pain along with hot flashes. Her clinician discusses HRT—not as a “miracle fix,” but as a tool that might ease several symptoms if risks are acceptable.
Key takeaway: HRT may only offer “partial relief, not complete reversal” for joint pain, so set expectations accordingly.
For anyone considering this path, the smartest move is to balance potential gains in daily comfort with the well-established risks, tailoring the decision with a qualified medical provider.
Who Should and Shouldn’t Consider Hormone Therapy for Joint Pain
Best Candidates for HRT
If joint pain started right as menopause symptoms kicked in, you’re in that classic target zone for hormone therapy.
The most likely candidates for HRT are:
- Women with new, widespread joint aches (called diffuse arthralgia) that appear around perimenopause
- People whose joint pain lines up with hot flashes, night sweats, or sudden sleep changes
- Anyone where tests have ruled out inflammatory, autoimmune, or mechanical causes of joint pain
- Folks already meeting HRT standards due to vasomotor or urogenital symptoms—think persistent hot flashes or vaginal dryness
Picture this: you’re usually fine, but as soon as your cycles start to change you wake up stiff, sore, and creaky, especially in the morning. If that sounds familiar—and other causes are ruled out—HRT may help dial down the discomfort.
“Women whose joint pain is timed with menopause and other classic symptoms may see real, if modest, benefits from HRT.”
When HRT May Not Be Appropriate
HRT isn’t for everyone, and knowing when to hit pause is just as valuable.
You’ll want to be cautious—or skip HRT entirely—if you:
- Have a history of breast cancer, unexplained vaginal bleeding, blood clots, or untreated high blood pressure
- Live with chronic joint pain that started well before menopause
- Have significant mechanical arthritis (like severe osteoarthritis) or a systemic inflammatory disease such as rheumatoid arthritis
- Are well past the “window of opportunity”—usually more than 10 years since menopause—when HRT risks outweigh benefits
It’s not just a checklist—it’s about context. Think of HRT as most effective for “menopausal joint pain,” not “all joint pain.” If pain’s older, severe, or due to another disease, you’ll want an alternative route.
“Not every joint ache after 40 points to menopause—matching the right therapy to the cause saves hassle and side effects.”
Let’s Make This Personal
Figuring out who fits: imagine someone age 52, who’s two years since her last period, suddenly waking up with aching fingers and knees, plus night sweats. If she’s otherwise healthy and has no major cardiovascular risks, she’s a classic candidate.
Contrast that to a woman with joint pain since her 30s, or who has a prior breast cancer diagnosis—HRT is unlikely to be suitable.
Early, data-supported conversations with your healthcare provider can make this process safer and far less frustrating.
The takeaway: HRT can offer meaningful relief—but it’s most effective, and safest, when used in the right person at the right time. Smart selection is your best ally for results.
Practical Approach to Using HRT for Menopausal Joint Pain
Stepwise Decision-Making: Laying the Groundwork
If you’re considering hormone replacement therapy (HRT) for menopausal joint pain, it pays to take a systematic approach—think of it as troubleshooting a tech issue, but for your health.
Start with:
- Ruling out other causes:
- Arrange for lab tests, imaging, or a specialist referral
- Exclude conditions like inflammatory arthritis, injury, or autoimmune disorders
- Assess your candidacy with your clinician:
- Review your age, medical and family history
- Consider the time since your last period and any comorbidities
- Set realistic expectations:
- HRT typically leads to partial—not total—relief
- Plan for symptom monitoring and ongoing reassessment
“Picture this: Tackling joint pain with HRT is like installing a much-needed update—helpful, but not a total system overhaul.”
Customizing Your HRT: Key Choices and Tips
You’ve decided HRT might help—how do you tailor it for maximum benefit?
Select your regimen:
- Systemic vs. local therapy: Systemic (whole body) is standard for joint symptoms; local is mainly for vaginal discomfort.
- Oral vs. transdermal: Transdermal (patch/gel) may cause fewer side effects for some women.
- Estrogen alone vs. combined therapy: You’ll need estrogen plus progestogen if you still have a uterus.
Practical optimization tips:
- Start low, go slow with doses and monitor for changes.
- Use a symptom diary or simple tracking app to log relief and side effects.
- Schedule regular check-ins for risk assessment and personalizing your plan.
“Customizing your hormone therapy is like optimizing your content workflow—you don’t hit publish without a review and adjustment.”
Supporting Strategies: More Than Just Hormones
HRT shines brightest when paired with a holistic approach. Even modest pain reduction makes way for bigger wins when you combine science-backed lifestyle choices:
- Exercise: Blend regular aerobic moves (like brisk walks) with strength training.
- Diet: Favor anti-inflammatory foods—think leafy greens, berries, and fatty fish.
- Weigh-in: Maintaining a healthy weight lightens your literal load on joints.
Adjunctive therapies can also help:
- NSAIDs (as needed for flare-ups)
- Physical therapy (especially for mobility)
- Complementary options like yoga or acupuncture
“Relief comes quicker with teamwork: HRT may be powerful, but it’s not meant to work alone.”
When you pull together targeted hormone therapy and lifestyle upgrades, you set yourself up for the best chance at comfortable, active days. For most, it’s the combo—not the quick fix—that delivers results worth sharing.
Current Trends, Controversies, and What’s Ahead
Hormone therapy (HRT) for menopausal joint pain is in the middle of a big transformation, with the latest data sparking both hope and questions for millions of women.
Picture this: Women in 2025 are discussing joint pain relief and menopause in virtual support groups, and clinical guidelines are now evolving based on major recent trials.
Evolving Guidelines and Fresh Evidence
Professional societies are updating recommendations as more real-world studies roll out. The latest clinical guidance:
- Supports HRT as an option for joint pain, especially when started within the “window of opportunity” (typically within 10 years of menopause).
- Recommends a stepwise evaluation to rule out inflammatory and mechanical arthritis before considering HRT.
New data shows that about 1 in 3 women experience significant improvement in joint aches with hormone therapy—but it’s not universal, and effect size varies.
Innovative Delivery Approaches and Dosing
Technology is shaking up the scene. Recent advances include:
- Transdermal patches and skin gels for more stable hormone levels and possibly fewer side effects than oral pills.
- Ultra-low-dose regimens aiming to deliver joint relief with minimized risk—a trend many experts are monitoring closely.
- Research is testing bio-identical formulations and “smart” dosing that adapts to a user’s cycle or symptoms.
Imagine slipping on a skin patch as easy as a smartwatch—and actually feeling your knees move more easily in the morning.
Unanswered Questions and The Road Ahead
There’s plenty left to figure out, including:
- Who truly benefits from HRT for joint pain—and who won’t notice much change?
- What are the long-term joint health outcomes of different regimens?
- How precise can we get—could future HRT be personalized using biomarkers or even AI to predict who responds best?
Experts agree on this: “Shared decision-making is here to stay.” Modern guidelines prioritize patient preferences and real conversations before starting HRT.
Looking Forward: What’s Next for Women and Providers
Expect larger, collaborative studies in the next couple years—plus more visibility for patient voices and advocacy groups.
- Look for more robust data on long-term safety and cost-effectiveness by 2026.
- Watch as real-world digital health tracking (think wearables) gets used to measure joint comfort and daily movement changes in response to therapy.
For now, if you’re considering HRT for joint pain, you’re not alone—global interest and innovation are at their highest point ever.
The bottom line: Hormone therapy for menopausal joint pain is evolving fast. Personalized, evidence-based choices and honest conversations with your healthcare team matter more than ever.
Conclusion
Addressing menopausal joint pain is about more than just easing discomfort—it's your opportunity to reclaim comfort, movement, and focus during one of life’s biggest transitions.
Navigating hormone therapy is no one-size-fits-all journey, but having the right information and a collaborative care plan fuels better choices. When you recognize your symptoms, know your options, and work with your provider, those creaky mornings can become your launchpad for newfound energy.
Take these actionable steps to move forward:
- Track your joint symptoms and patterns—bring notes to your next clinician visit for a targeted conversation
- Rule out other causes first before considering hormone therapy, ensuring your approach matches your needs
- Ask about HRT if your joint pain started or worsened with menopause, especially if hot flashes and sleep changes joined the party
- Start low and adjust slowly with any new regimen—monitor your response and side effects using a simple diary or tracking app
- Combine HRT with proven lifestyle strategies: prioritize regular movement, a joint-friendly diet, and daily routines that support overall well-being.
Ready to take action? Reach out to your healthcare provider and start a focused, open dialogue about personalized joint pain solutions. Equip yourself with specifics—symptom logs, questions about risks and benefits, and a willingness to explore the right timing for treatment.
Stay tuned for new advances in hormone therapy and digital health tools—because joint pain relief is evolving, and you deserve support that keeps up with your goals.
You don’t have to let menopause write your story—take the wheel, make informed choices, and get back to moving freely. Relief isn’t just possible; it’s worth pursuing.