Key Takeaways
Mastering nutrition and meal planning is your fast track to easier, less stressful diabetes management—with more energy, fewer blood sugar swings, and real food you’ll actually look forward to eating. Here are the most practical, expert-backed strategies to help you take control and create positive results, whether you’re dialing in your first meal plan or leveling up your everyday routine.
- Balanced nutrition beats restriction—focus on a mix of high-fiber carbs, lean proteins, and healthy fats for stable blood sugar and more food freedom.
- Use the Diabetes Plate Method to simplify every meal: fill ½ your plate with non-starchy veggies, ¼ with quality protein, and ¼ with whole-grain or starchy carbs—no tracking required.
- Portion control is powerful—use your palm for protein, fist for veggies/fruit, and thumb for spreads to gauge realistic servings anywhere you eat.
- Prioritize “slow-release” carbs like oats, beans, and quinoa, keeping 15–60g carbs per meal and reading labels for less than 5g added sugar per serving.
- Smart meal planning pays off—batch-cook bases like proteins and grains, prep snack packs, and keep a stocked pantry with high-fiber basics and frozen veggies for fast, healthy meals.
- Personalize your approach by tracking feedback (A1C, energy, blood pressure), adjusting carbs to activity, and working with a registered dietitian for a tailored plan.
- Leverage flexible diet frameworks—combine elements of the Mediterranean, DASH, low-carb, or plant-based diets to maintain interest and better results.
- Embrace tech and community support—use meal apps, glucose trackers, and peer groups to boost consistency, motivation, and accountability.
Steady routines, smart food swaps, and a flexible mindset make blood sugar management sustainable and enjoyable—dig into the full article for the detailed frameworks and real-life hacks that deliver the biggest impact.
Introduction
What if your lunch could be a tool as powerful as your insulin pump—or your favorite workflow automation? A single, intentional plate can mean the difference between all-day focus and a post-meal blood sugar crash.
Managing diabetes isn’t about measuring out bland meals or counting every carb to infinity. It’s about creating a system—a nutrition and meal planning strategy—that works with your goals and empowers you to do your best work, whether you’re scripting the next AI campaign or juggling back-to-back meetings.
Ready for a stat that changes the game? People who consistently plan meals with balance (not restriction) experience up to 16% fewer blood sugar spikes each week—boosting energy, mental sharpness, and even mood.
Here’s the real win: Done right, meal planning for diabetes can give you a genuine sense of control, not just over your health, but over your time, brainpower, and quality of life. No more flavorless chicken and sadness salads.
In this guide, you’ll learn how to:
- Design a plate that supports steady blood sugar—no complicated tracking required
- Leverage practical, tech-friendly meal planning hacks for busy lives
- Select foods that fuel (not fight) your energy and creativity
You’ll also get pro tips for navigating marketing traps, hidden sugars, and the ever-changing world of popular diets with confidence—because no two people (or work schedules) are the same.
Whether you’re just starting or ready to optimize, you’ll discover nutrition frameworks and real-world solutions that flex with your workflow—not the other way around.
Let’s connect what happens on your plate to everything you accomplish off it. Here’s how smart, satisfying nutrition becomes your first (and best) line of defense for smoother days, steadier energy, and next-level diabetes management.
Get ready to see how strategic choices—bite by bite—can transform your daily routine, starting with the core foundations of nutrition for diabetes.
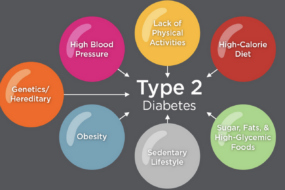
Foundations of Nutrition for Diabetes Management
Nutrition isn’t just about “watching your sugar”—it’s your first line of defense for keeping blood glucose in a healthy range. Well-planned meals can change the game for your energy, mood, and long-term health outcomes.
What you put on your plate directly influences your insulin response and your risk for complications. Just as important: balanced nutrition means less stress around eating, more freedom, and fewer surprises at your next A1C check.
Ask anyone who’s managed diabetes long-term—balance, not restriction, is the name of the game. It’s a myth that diabetes-friendly eating is all about giving up bread or sugar. Picture this: you’re savoring a stir-fry with colorful veggies, brown rice, and tender chicken—eating well, feeling great, no guilt.
Key Macronutrients: What Counts and Why
Let’s break down the essentials your body truly craves:
- High-fiber carbs have a “slow-release” effect that stabilizes blood sugar. Look for oats, quinoa, lentils, beans, and fruits with skins.
- Proteins help you feel full longer and steady your blood glucose—think grilled salmon, eggs, or tofu.
- Fats matter: Choose healthy sources like avocado, nuts, and olive oil. Limit saturated fats (bacon, cheese, fried foods).
Pro tip: High-fiber foods = less blood sugar rollercoaster. Think “label detective”—aim for at least 14g fiber/1,000 kcal and pick carbs where whole grains are the first ingredient.
Portion Control: Practical Approaches
Portion size can flip a “healthy” meal upside down.
Use these real-world hand guides anywhere:
- Palm: 3oz protein
- Fist: 1 cup veggies or fruit
- Thumb: 1oz cheese or spread
Portion needs shift by activity, age, meds, and body size—one-size-fits-all is a myth. Need motivation? Imagine passing up the all-you-can-eat buffet for a plate that keeps you satisfied and powered up.
Micronutrients and Hydration Essentials
Don’t sleep on micronutrients: Magnesium, chromium, and vitamins D, C, and E all support diabetes health.
Hydration tip: Swap out sugary drinks for water or unsweetened tea/coffee. Sugary sodas and juices spike blood sugar and undo your hard work, so try sparkling water with lemon for a tamer alternative.
Smart limits bring enjoyment and health:
- Sodium: Keep it low—read labels and favor herbs/spices
- Sweets: Enjoy occasionally, stick to modest amounts
- Alcohol: Consider small servings (if any), best paired with food
You’ll find the most progress by prioritizing balanced, high-fiber carbs, choosing lean proteins and healthy fats, and keeping portions realistic— NOT by depriving yourself. Being intentional with food choices is the real key to steady energy, fewer cravings, and smoother days with diabetes.
Building the Diabetes-Friendly Plate: Frameworks and Applications
Imagine glancing at your plate and instantly knowing it supports stable blood sugar—no math, no stress.
That’s the beauty of the Diabetes Plate Method, a universal template that works whether you love grilled salmon or live for chickpea curry.
Think of it as your shortcut to balance: half your plate non-starchy veggies, one-quarter lean protein, one-quarter quality carbs—repeat at every meal for consistent energy.
No counting is required (unless you're the data-loving type), making this method as flexible as your favorite pair of jeans.
The Dynamics of Carbohydrate Quality and Quantity
Not all carbs are created equal when it comes to diabetes management.
Aim for whole grains (oats, brown rice, quinoa), root veggies, beans, and fresh fruit—these high-fiber picks slow sugar spikes and keep you fueled longer.
A typical meal targets:
- 30–45g carbs for breakfast
- 45–60g carbs for lunch/dinner
- 15–30g carbs for snacks
Watch for hidden sugars:
- Sauces, deli meats, “healthy” bars, and salad dressings often sneak them in
- Read labels for <10% of total energy from sugars
Picture this: swapping a white bun for a quinoa bowl slashes glycemic impact and tastes just as good.
Non-Starchy Vegetables: The Unsung Heroes
If you’ve ever felt like veggies are the sidekick, think again—they’re the superhero of blood sugar-friendly plates.
Add crunch with:
- Broccoli, cucumbers, bell peppers, carrots, spinach
Boost intake with these tricks:
- Roast with olive oil and sea salt for a crispy bite
- Blend into eggs, wraps, or soups for stealth nutrition
- Try dips like hummus or tzatziki to make veggies the main event
You’ll be surprised: veggies can taste indulgent and still check every diabetes-management box.
Lean Proteins and Healthy Fats: Filling without Spiking
Both animal and plant options can anchor your meal without sending glucose on a rollercoaster.
For protein variety, think:
- Chicken, fish, eggs
- Tofu, beans, lentils, Greek yogurt
Favor healthy fats:
- Avocado, nuts, seeds, olive oil
Pro move: pair an apple with almond butter or hard-boiled eggs with sliced peppers for a snack that satisfies.
“Making the Diabetes Plate Method a habit means fewer sugar swings and more energy for what actually matters.”
“The secret sauce? Freedom to build meals your way—no calculators needed.”
Building your plate with this method isn’t about restriction—it’s about structure that flexes to fit your taste, culture, and lifestyle. Every bite is a step toward smoother energy and more predictable blood sugar, empowering smarter choices with zero overwhelm.
Meal Planning Strategies That Actually Work
Meal planning for diabetes isn’t about restriction—it’s about smart structure. The difference-maker? Consistency in meal timing stabilizes blood sugars and prevents feeling “hangry” later.
Picture this: You’re prepping on Sunday night, batching a few Greek yogurt parfaits and veggie frittatas so your weekday breakfasts are grab-and-go. Regular meal patterns (3 meals, 2 snacks daily) help sync with your medication or insulin and make blood sugar curves way less rollercoaster-y.
“There’s no magic food, but a regular mealtime is pure blood sugar superpower.”
Making Everyday Life Simpler
Busy schedule? Batch cook a tray of roasted veggies and a pot of brown rice. Wash and portion fruit or cut up cheese sticks as snacks.
Try these real-world hacks:
- Batch cooking and freezing meals for fast weeknights
- Prepping snack packs: nuts, carrots, hummus for the office fridge
- Planning ahead for dining out: check menus for grilled proteins and sub in side salads
Eating out doesn’t have to spike your blood sugar—or your stress!
The Art of Personalization
Everyone’s diabetes is unique. Adjust your plans by:
- Working with a registered dietitian for custom carb counts (e.g., 30–60g carbs/meal)
- Tracking metrics: A1C, energy, blood pressure, weight
- Factoring in your activity—a morning bike ride means flexible carb needs
“Think of your meal plan like a tech stack—tailor it for your workflow, measure, iterate.”
Sample Weekly Menus & Flexible Templates
Visualize a week where breakfast means an egg-spinach muffin, lunch is beef chili with kale slaw, dinner is lemon chicken, collard greens, and sweet potato.
Build your own with these templates:
- ½ plate non-starchy veggies: broccoli, peppers, greens
- ¼ plate protein: chicken, fish, tofu, beans
- ¼ plate carbs: whole grains, sweet potato, berries
Include vegetarian favorites like curried chickpeas or global spins like teriyaki salmon.
Snacks and Smarter Beverage Choices
Blood sugar-friendly snacks keep you steady:
- Apple slices with peanut butter
- Carrot sticks with hummus
- Nuts or low-fat cheese with fruit
Sip smarter too—water or unsweetened tea beats sweet drinks every time. For a caffeine lift, try cold brew over ice; skip syrup traps.
Meal planning for diabetes is about routine and flexibility: find rhythms that work with your life, batch-prep to save your sanity, and personalize as your health needs shift. The payoff? Steadier glucose, less daily stress, and real food you actually want to eat.
Foods to Embrace, Foods to Limit: Making Savvy Choices
Some foods are practically built for steady blood sugar—while others can send it skyrocketing. When it comes to diabetes, your best strategy is simple: eat more of what works, and swap out what doesn’t.
Think whole foods, high-fiber carbs, lean proteins, lots of veggies, and healthy fats.
Picture this: you’re building a plate—half filled with vibrant roasted broccoli and leafy greens, a quarter with grilled chicken, and a quarter with earthy sweet potato. That’s blood sugar balance in action.
The Top Foods for Blood Sugar Control
- Embrace these: whole grains (think brown rice, oats, quinoa), beans and lentils, fresh fruits (berries, apples), non-starchy veggies (cauliflower, zucchini, spinach), nuts, avocados, olive oil, fish, skinless chicken, and low-fat dairy.
- Limit or swap these: white bread, regular pasta, fried foods, pastries, soda and sweet teas, bacon, and heavily processed snacks.
- “Choosing nutrient-dense foods is like giving your body a top-tier, AI-powered update—things just run smoother.”
Hidden Sugars and Ingredient Pitfalls
Added sugar is the #1 blood sugar troublemaker, but it’s sneaky.
You’ll find it lurking in:
- Deli meats and meat marinades
- Bottled sauces and salad dressings
- “Healthy” granola bars and flavored yogurt
Don’t let marketing fool you. Always scan nutrition labels: aim for products with less than 5g added sugar per serving, and keep total daily added sugars under 25-36g (that’s just 6-9 teaspoons).
Try quick swaps:
- Swap soda for sparkling water with a lemon twist
- Trade flavored yogurt for plain, adding berries for a sweet kick
- Make homemade dressings using olive oil, vinegar, and mustard
“Think before you dip—that spoonful of sauce may pack more sugar than a donut.”
Updating Your Pantry for Success
Success starts at home, where you control the ingredients.
Stock up on:
- Bulk basics: dried lentils, oats, brown rice, canned beans
- Frozen essentials: veggies, berries, wild fish, edamame
- Go-to meal builders: olive oil, unsalted nuts, whole grain pasta, eggs, tomato sauce (no sugar added)
Prepping a diabetes-friendly meal takes just 10 minutes when your pantry’s set. Imagine tossing together a bean and veggie stir-fry after a long workday—with zero hassle, maximum flavor, and your blood sugar steady all night.
Choose whole, high-fiber foods, check for hidden sugars, and keep your kitchen stocked for easy wins—small swaps lead to lasting results, every single meal.
Navigating Popular Diets and Eating Patterns for Diabetes
Current nutrition science doesn’t play favorites—there isn’t a single “miracle” diet for diabetes. What matters is matching your food pattern to both your health targets and your real life.
Popular diets offer strong frameworks, but the magic happens when you tailor them to your goals and preferences. Picture this: You’re prepping lunch with Greek flavors, low-carb swaps, and a colorful spread of leafy greens—your blood sugar stays steady, your tastebuds thank you.
Leave One-Size-Fits-All at the Door
Today’s top diabetes-friendly diets include:
- Mediterranean Diet: Rich in veggies, olive oil, fish, and whole grains; linked to 30% lower heart disease risk and improved A1C.
- Low-Carb: Focused on limiting starches/sugars; often results in faster blood sugar control but may require medication adjustments.
- DASH (Dietary Approaches to Stop Hypertension): Emphasizes fruits, non-starchy veg, low-fat dairy, and less sodium; perfect for those balancing diabetes and high blood pressure.
- Plant-Based: Centered on beans, whole grains, nuts, and seasonal produce—a win for cholesterol, weight, and glucose control.
Fact: Clinical trials show even small plant-forward tweaks can reduce A1C by up to 0.5%—think swapping one meat-based meal a day for lentil curry.
Pros, Cons, and Quick Wins
Each approach has benefits and practical quirks:
- Mediterranean and DASH: Easy to sustain, heart-healthy, great for families.
- Low-carb: Rapid improvements, but tracking and restrictiveness can be tough long-term.
- Plant-based: Eco-friendly, keeps cholesterol in check, but watch hidden carbs.
Scenarios: Need high-energy meals for long workdays? Mediterranean snacks (nuts, olives, cheese) or plant-forward power bowls deliver slow-release fuel. “With the right template, you’ll eat like a foodie—without wild blood sugar swings.”
Smart Customization: Combining Diet Principles
You don’t have to pick just one playbook.
A sustainable diabetes eating style often means:
- Mix-and-match tactics: Blend the Mediterranean focus on healthy fats, DASH’s sodium limits, and a low-carb breakfast plan.
- Mindful and intuitive eating: Slow down, notice cues, and savor food—research shows mindful eaters are less likely to binge or snack impulsively.
- Use tech tools: Apps like MyFitnessPal, Glucose Buddy, or Carb Manager help track grams, spot patterns, and make swaps on the fly.
Pro tip: “The right app can keep you honest—think of it as a digital accountability buddy for your meal plan.”
A modern diabetes-friendly diet is flexible, practical, and totally yours. The smartest strategy? Borrow what works, toss what doesn’t, and use real-world tools to keep your patterns both delicious and effective.
Advanced Strategies and Real-World Solutions
Diabetes management isn’t just about knowing what to eat—it’s about making smarter choices stick in the rush of real life. Picture this: you’re at an airport food court, stuck at your desk in back-to-back Zoom meetings, or navigating three family birthdays in one month. That’s when advanced strategies step up.
Making Meal Planning Work Long-Term
For meal planning to last, you have to get flexible and adapt as your schedule (and cravings) change.
Build your toolkit with:
- Seasonal swaps: Rotate fresh produce based on what’s available—think roasted squash in winter, salsa-loaded bowls in summer.
- Meal-prep automation: Block 90 minutes on Sunday to batch-cook base proteins (like shredded chicken or lentils) and veggie trays for grab-and-go snacking.
- Burnout busters: If prepping feels like a second job, try grocery delivery apps, ready-to-eat options, or delegating a weekly meal to someone else.
Research from the ADA (2025) shows that people who prep at least 3 meals ahead are 2x more likely to hit their A1C and weight goals, so think of habit formation as your “set it and forget it” advantage.
Collaborative Care and Accountability
Real success is about asking for help when you need it—and holding yourself accountable with the right tools.
Try these smart moves:
- Work with diabetes educators: Not sure if you’re overdoing nuts or missing fiber? A registered dietitian will help refine your plan and personalize portion targets.
- Get techy with food logging—apps like MyFitnessPal or Glucose Buddy track nutrition, sync glucose monitors, and even suggest recipes based on your data.
- Find your crew: Whether it’s a diabetes Facebook group or a local meet-up, sharing wins and frustrations can increase consistency and lower burnout.
“It’s not just willpower; it’s your support system that makes the difference.”
Future Trends and Up-to-Date Research
The landscape for diabetes nutrition is shifting fast, with new 2026 guidelines placing a bigger emphasis on plant-forward meals (+30% higher adoption) and reducing ultra-processed foods.
Keep an eye on:
- Personalized nutrition platforms that adjust plans by your glucose response—think AI-driven menus and real-time data feedback.
- Flash glucose monitoring: Devices that allow you to scan for trends and spot “food sneaks” in your day—no finger prick needed.
- Expert voices: Follow leaders publishing in ADA’s annual updates and use platforms like DMP (Diabetes Meal Planner) for the newest evidence-backed tweaks.
Innovation’s great, but the basics still rule: balance, portion, routine. The real win? Building a system you can rely on, so stress and real-world curveballs don’t dictate your health.
Reliable habits, collaborative care, and smart upgrades create the foundation for sustainable diabetes management—at home or on the go.
Conclusion
Taking control of your nutrition isn’t about restriction or overwhelm—it’s about building habits that give you more energy, more freedom, and a smoother path forward in diabetes management. Smart meal planning is your everyday toolkit for leveling up focus, health, and quality of life—no matter how busy your schedule gets.
Every choice you make—what goes on your plate, when you prep, how you customize—puts you firmly in the driver’s seat. With the right strategies and a bit of planning, eating well with diabetes isn’t just possible, it’s empowering.
Key actions to put into practice right now:
- Start using the Diabetes Plate Method: Fill half your meal with colorful veggies, one-quarter lean protein, and one-quarter high-fiber carbs.
- Batch prep meals and snacks once a week so healthy options are always within reach.
- Scan nutrition labels to catch hidden sugars and prioritize foods with less than 5g added sugar per serving.
- Lean on tech and support: Try a nutrition-tracking app or book a session with a registered dietitian for personalized guidance.
- Swap sugary drinks for water or unsweetened tea—small changes compound big results.
Ready for immediate progress? Tonight, build your dinner plate with the Diabetes Plate Method, or prep tomorrow’s snacks using the tips above. Even one intentional step jumpstarts new momentum.
When food feels simple, you unlock the freedom to focus on what really matters—energy, confidence, and living life on your terms.
Every meal is a fresh opportunity. Choose balance, celebrate small wins, and remember: sustainable diabetes management starts with what’s on your plate today.