Key Takeaways
Looking to slash joint inflammation and boost everyday comfort? These core strategies distill expert guidance into quick, actionable steps—so you can start reducing pain and swelling without wading through medical jargon. Here’s how to turn the science into daily wins for your joints.
- Recognize lingering swelling as a signal, not background noise—persistent joint pain or heat means your body wants support, not just rest.
- Jumpstart recovery with the RICE protocol—Rest, Ice, Compression, and Elevation are the go-to steps for fast relief during acute flare-ups.
- Choose ice for new swelling, heat for stiffness—ice calms red, inflamed joints, while gentle heat is best saved for ongoing tension (not active swelling).
- Fuel your joints with an anti-inflammatory diet—omega-3-rich fish, leafy greens, and berries actively reduce inflammation, while processed foods and sugar crank it up.
- Move smarter with low-impact exercise—walking, cycling, swimming, and yoga help lower inflammation and preserve joint function, even if you start with micro-bursts.
- Stress less, sleep more to calm inflammation—chronic stress and poor sleep ramp up joint pain, so add mindfulness or a consistent bedtime to your toolkit.
- Leverage proven meds (NSAIDs, DMARDs) and real supplements—use NSAIDs and topical creams for immediate relief, and talk to your clinician before trying fish oil or turmeric.
- Track patterns and personalize your plan—logging symptoms and triggers lets you pinpoint what works and partner effectively with your doctor for tailored strategies.
Ready to turn these quick wins into lasting comfort? Dive into the full article for practical tips, smart swaps, and data-driven decision-making to keep your joints moving strong.
Introduction
Ever felt a sharp, stubborn ache in your knee after a long workday—only to have it flare up again during your next Zoom marathon?
You’re not alone: 1 in 4 adults deal with joint pain or swelling each year, and in fast-moving careers, those aches don’t just slow you down—they steal focus, sap productivity, and make everyday tasks feel like uphill sprints.
If you’ve ever wondered why your “tech neck” morphs into sore shoulders, or why your post-pickleball hips feel twice as old as your LinkedIn profile, you’re in smart company.
Inflammation isn’t just background noise, and ignoring it rarely makes it better.
But here’s the good news: you can dial down joint inflammation using a blend of real-world strategies—no fad cures, no unrealistic promises.
In this guide, you’ll get:
- Instant, actionable relief tactics for sudden flare-ups (because deadlines don’t wait for swollen wrists)
- Diet hacks that help turn down the heat—think omega-3s, antioxidant-rich foods, and practical food swaps, all with a busy schedule in mind
- Evidence-based supplements and medications—and which ones are worth your attention (and your wallet)
- Lifestyle upgrades proven to cut inflammation, like micro-bursts of movement, stress management tricks, and smarter sleep routines
- Guidance on when expert input matters—so you know exactly when to escalate, not just “tough it out”
The goal isn’t to overwhelm you with biology or force a radical lifestyle overhaul. Instead, you’ll grab the exact toolkit you need—one you can tweak, automate, and track (hello, habit apps and wearable data) to support your career, hobbies, and everyday comfort.
Ready to spot what’s driving your joint symptoms and put practical, proven solutions to work—without missing a beat?
Let’s unravel what’s really behind persistent swelling and lay out the straightforward fixes that actually make a difference.
Understanding Joint Inflammation: Causes and Why It Happens
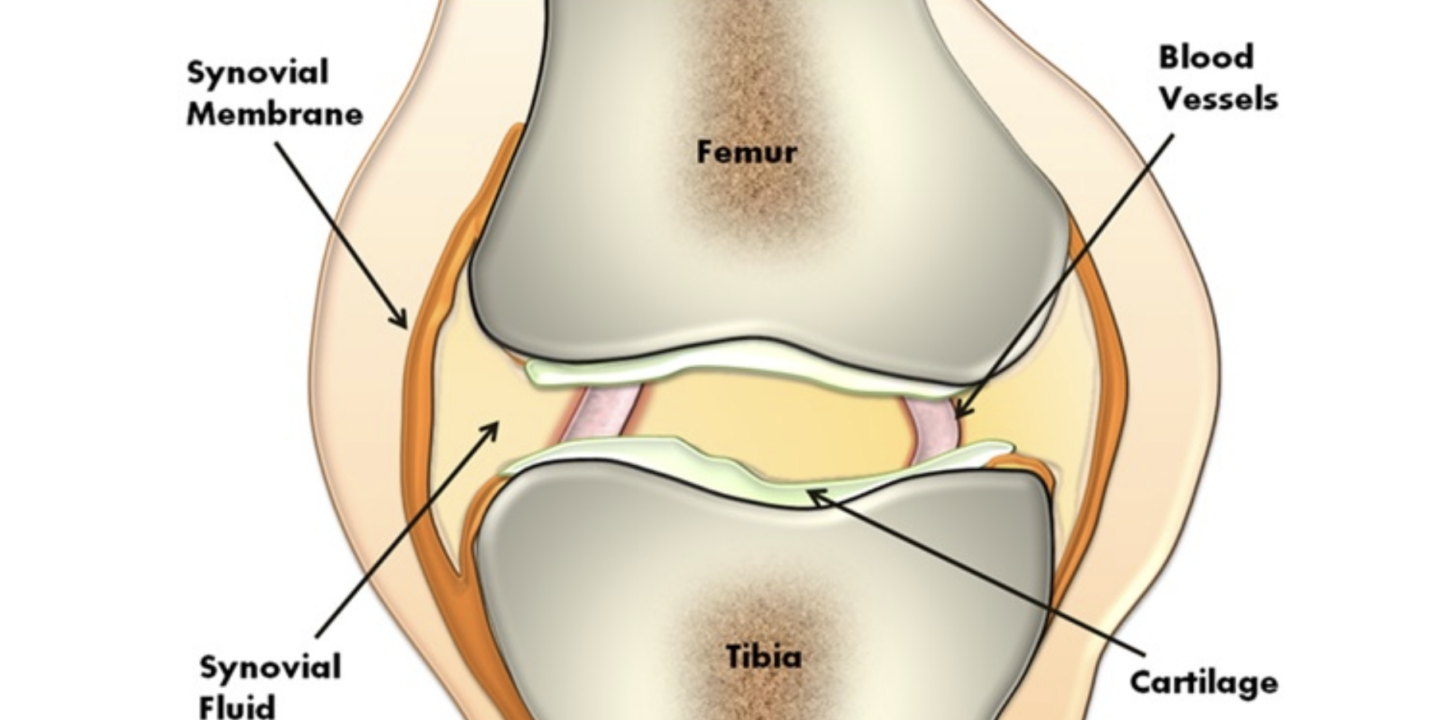
Joint inflammation, in simple terms, is when your body’s immune system sends fluids and immune cells to a joint, making it swollen, tender, or warm.
Think of it as your biological “repair crew” showing up—sometimes for good reason, sometimes by mistake.
But when that swelling lingers, it’s not just annoying: it’s your body’s way of waving a red flag, signaling that something deeper needs attention.
What Are the Most Common Types of Joint Inflammation?
You’re not alone if you’re tackling joint swelling—nearly 1 in 4 adults in the U.S. reports arthritis or joint pain.
The main culprits include:
- Osteoarthritis: Wear-and-tear over years causing cartilage breakdown—picture creaky knees after a long walk or stiff hips waking up.
- Rheumatoid arthritis: The immune system attacks joint linings, leading to unpredictable flare-ups and deeper aches.
- Gout: Sharp uric acid crystals form in the joint (think: a sudden, throbbing big toe).
- Injury-related inflammation: From sprains, overuse, or even an awkward twist on the pickleball court.
Under the Hood: What Triggers Inflammation?
The mechanics look like this:
- Immune response: White blood cells flood a joint to fight off supposed threats, even if there’s no real invader.
- Wear-and-tear: Years of movement (or one bad injury) whittle down cushioning, letting bones rub—causing swelling and pain.
- Crystals or debris: Tiny irritants (like uric acid crystals in gout) fire up local inflammation.
Picture this: a swollen finger after gardening, or a heat-red knee after an intense Peloton session—that’s inflammation in action.
Why Managing Inflammation Matters—Beyond Just Pain
Untreated inflammation does more than nag at you—it can:
- Limit mobility and sap productivity (joint stiffness often steals an hour of movement when you wake up)
- Trigger long-term damage: Studies show persistent swelling can lead to bone loss, joint deformity, and weakened muscles
One sharable truth: “Persistent swelling isn’t just background noise—it’s your body asking for support.”
When you spot swelling, pain, or warmth in a joint, see it as useful data, not just discomfort.
Learning what drives your symptoms is the first step to protecting comfort and mobility for years to come.
Quick Relief Strategies for Acute Joint Swelling
When your joint suddenly swells, feels hot, or is sharply painful, you need fast relief—think of this as a fire drill for your body.
Acute swelling is your body’s SOS—and your top priority is to calm things down and prevent further damage.
What should you do first? Let’s break it down for those moments when every minute counts.
RICE Protocol: Four Steps to Immediate Relief
The classic RICE protocol is the gold-standard for new or flaring joint swelling—don’t overthink it, just act:
- Rest: Take the pressure off (skip the gym, text a friend to pick up your coffee).
- Ice: Apply something cold—yes, even a bag of frozen peas—for 10–20 minutes every 2 hours.
- Compression: Use an elastic bandage (but not so tight it cuts off circulation).
- Elevation: Prop the joint above heart level—picture binge-watching your favorite show with your ankle on a pile of pillows.
Quotable tip: “Think of RICE as your go-bag for joint emergencies—fast, reliable, and ready-to-use.”
Ice vs. Heat: When to Chill and When to Warm
Not sure if you should reach for the ice pack or a heating pad?
- Use ice: For swelling, redness, or after an injury/flair. It reduces blood flow and inflammation.
- Use heat: For lingering stiffness (not fresh swelling!). A warm shower or pad loosens tight muscles, but skip heat if your joint is hot and swollen.
Visual moment: Picture gently pressing an ice pack to a puffy red knee versus relaxing your hands around a warm mug after morning stiffness.
Topical Relief: Fast-Acting Creams and Gels
You can find over-the-counter creams, gels, or patches at most pharmacies, often containing:
- NSAIDs (like diclofenac gel): Reduce both pain and inflammation, with fewer whole-body side effects.
- Menthol or capsaicin: Create a cooling or warming sensation that distracts from pain; good for mild cases, but don’t expect miracles.
Skip herbal “cure-alls”—evidence is weak and results are inconsistent.
When to Call a Clinician: Red Flag Symptoms
DIY isn’t enough if you spot:
- Red, very hot, or severely painful joints
- Swelling that lasts more than a few days
- Multiple joints involved, fevers, or feeling unwell
Early help means better outcomes. “Don’t tough it out if your joint looks angry—consult a pro.”
Acute flare-ups demand rapid, smart action: start with RICE, choose ice over heat for big swelling, and use proven creams for quick relief. If symptoms persist or escalate, reach out to a clinician—your long-term joint health depends on it.
Anti-Inflammatory Diet Choices for Joint Comfort
When it comes to joint comfort, your diet can make a real difference—sometimes faster than you think.
Decades of research show that certain foods actively turn down the dial on inflammation, while others crank it up. Think of your plate as a toolkit for supporting your joints every day.
Omega-3 Rich Foods: Your Joint Allies
Omega-3 fatty acids pack a powerful anti-inflammatory punch.
- Salmon, mackerel, and sardines: Just two servings a week can help reduce joint pain and swelling, according to studies in people with rheumatoid arthritis.
- Chia seeds and walnuts: Plant-based omega-3s are linked to fewer inflammatory flares—perfect for desk snacks or breakfast boosts.
Picture this: a vibrant quinoa salad with salmon, walnuts, and baby spinach. It’s delicious, nourishing, and secretly anti-inflammatory.
“Think of every bite as a micro-investment in your joint future.”
Antioxidant Heroes: Nature’s Chill Pill
Color is your friend here—vivid foods fight inflammation hardest.
- Leafy greens (spinach, kale)
- Deep-hued berries (blueberries, cherries, blackberries)
- Nuts, whole grains, and legumes
Fiber and antioxidants in these foods can significantly “cool” inflamed joints, lowering markers seen in blood tests.
“Berries and greens bring more than flavor—they bring joint comfort by the forkful.”
Sabotage Foods (and What to Swap)
Certain foods push inflammation into high gear, so keep these on your radar:
- Processed snacks and fast food
- Added sugar (think soda, cookies, sweetened cereals)
- Red meat and processed meats
- Trans fats (often found in fried and packaged foods)
Ready for an easy upgrade?
- Swap soda for infused water or green tea
- Opt for grilled fish instead of bacon or sausage
- Use olive oil and lemon for dressings—instead of creamy, packaged sauces
Spices with a Side of Real Talk
Turmeric and ginger get plenty of buzz, with modest research support for joint stiffness relief.
Sprinkle turmeric into soups and curries, or steep ginger in tea. But keep expectations realistic—these spices are best as tasty additions, not miracle cures.
What you eat today shapes how you move tomorrow. Fill your plate with omega-3s, vibrant plants, and whole foods to stack the odds in your joints’ favor—one meal, one snack, one smart swap at a time.
Lifestyle Shifts That Lower Inflammation Load
Joint health is about much more than what’s on your plate.
The habits you build outside the kitchen have a major impact on inflammation—sometimes more than diet alone. Simple adjustments to daily routines can reduce swelling and keep your joints moving comfortably, long-term.
Picture this: even losing 5–10% of your body weight can take serious pressure off your knees and hips, lowering inflammation markers throughout your body. Studies show the payoff is both physical and measurable—improved function, less pain, and a lighter inflammatory load.
Move Smart: Exercise Strategies That Work
Not all movement is created equal.
Low-impact activities cool down inflammation and build joint resilience over time.
Try adding these joint-friendly exercises:
- Walking briskly (even 10 minutes at a time counts)
- Cycling (indoor or outdoor)
- Swimming or water aerobics
- Yoga and stretching routines
If you’re thinking, “What if it hurts just to move?”—you’re not alone.
- Start small with chair-based stretches or mini-walks around the house
- Work with a physical therapist who tailors exercises to your situation
- Water exercise cushions every step, making it easier on painful joints
You don’t need fancy gear or an expensive gym—micro-doses of movement throughout your day add up fast.
Mind Meets Body: Stress Less, Sleep More
Here’s a surprising twist: mental health and joint inflammation are directly linked.
Chronic stress and lack of sleep trigger spikes in inflammatory chemicals in your body, often making joint pain worse.
Action steps:
- Try mindfulness meditation—just 5 minutes can help
- Practice relaxation breathing or progressive muscle relaxation at your desk
- Set a consistent sleep schedule and cut blue light (hello, late-night scrollers!) to help your body repair
“A calmer mind really can mean calmer joints.”
Smart lifestyle tweaks—shedding even a little weight, moving gently but consistently, and managing stress—work together to dial down joint inflammation. Think of your daily routine as your low-tech tool kit for lasting comfort and freedom of movement.
Strategic Use of Medications and Supplements
When you want to knock down joint inflammation quickly and effectively, knowing which treatments actually work is half the battle.
Medications like NSAIDs, corticosteroids, and certain disease-modifying drugs (DMARDs) have the strongest track records for reducing real inflammation—not just masking pain.
Picture this: After a tough pickleball match, your knee’s swollen, stiff, and red. If resting and icing don’t cut it, reaching for an NSAID (like ibuprofen or naproxen) can help with both pain and swelling.
But remember—regular use of NSAIDs can raise your risk of stomach ulcers, high blood pressure, and kidney issues. If out-of-the-bottle isn’t helping after a few days, that symptom deserves a check-in with your clinician.
When Each Medication Makes Sense
- NSAIDs: OTC or prescription, best for short‑term flares, watch for GI/kidney risks
- Corticosteroids: Pills or joint injections, powerful but for limited use due to side effects (think: weight gain, mood swings, immune changes)
- DMARDs (traditional and biologic): For conditions like rheumatoid arthritis or psoriatic arthritis; these slow actual disease—not just symptoms—and require specialist guidance
Topical creams, gels, and patches (think: diclofenac gel, menthol rubs) deliver relief right to the joint with far fewer whole‑body side effects than pills.
Supplements: What’s Real, What’s Hype?
Curious about the vitamin aisle? Here’s where the evidence lands:
- Fish oil (EPA/DHA): Doses of 600–1,000 mg/day can shave off joint pain and swelling, especially for rheumatoid arthritis, according to multiple studies
- Turmeric/curcumin and ginger: Have modest anti‑inflammatory effects; some benefit in chronic pain, but not a replacement for prescribed meds
- Glucosamine + chondroitin: Results are mixed; worth a trial for osteoarthritis if your doc gives a green light, but savings might be as helpful as supplements
Always consult your clinician before starting a supplement—fish oil can thin the blood, turmeric interacts with certain meds, and not all claims are created equal.
The Actionable Next Step
Picture scanning that pharmacy shelf, wondering: pill or patch? Capsule or curry spice? The smartest move is matching your approach to your condition and overall health, keeping side effects and interactions top of mind. Setting realistic expectations is your friend: “Supplements can support, but they rarely replace, proven medications.”
Knowing when and how to combine medications, topicals, and carefully chosen supplements gives you the best shot at lasting, targeted relief—with fewer unpleasant surprises along the way.
When to Get a Professional Opinion: Signs You Shouldn’t Ignore
Recognize Serious Joint Inflammation: Red Flags
Sometimes, joint pain is a sign your body needs urgent help—not just rest or an ice pack.
If you notice any of these symptoms, call your doctor or a specialist right away:
- Swelling that lasts more than 3 days or keeps coming back
- Multiple joints suddenly painful or stiff
- Redness, heat, or a joint that’s so tender you can’t touch it
- Severe pain at rest, especially at night
- Fever, chills, unexplained fatigue, or weight loss
- Trouble using the joint, or inability to bear weight
Picture this: If your knee is hot, red, and swollen for days, or your hands hurt so much you can’t type or grip your coffee mug, it’s time to move past home remedies.
“Lingering swelling and pain mean your joints are asking for backup—don’t wait for things to resolve on their own.”
What Happens at the Doctor’s Office
A specialist won’t just glance and guess—expect a thorough evaluation to pinpoint what’s going on.
This typically includes:
- Careful physical exam (looking for swelling, warmth, range of motion)
- Blood tests (checking for signs of inflammation, autoimmunity, or infection)
- Imaging such as X-rays, ultrasound, or MRI to see inside the joint
If you show signs of inflammatory arthritis, gout, or infection, you’ll get targeted treatment—often within days.
“The faster you get answers, the sooner you can avoid joint damage and get relief.”
Advanced Solutions: What If It’s More Serious?
For tough or chronic cases, your care team might recommend:
- DMARDs or biologic drugs (these suppress rogue immune activity for RA and similar diseases)
- Joint injections (corticosteroids or hyaluronic acid provide rapid, targeted relief)
- Surgical procedures (like joint replacement for advanced damage—typically after other therapies)
Current guidelines say early intervention saves joints—and your long-term mobility.
A persistent red or swollen joint is more than an inconvenience—it’s a signal to act. If your pain is severe, spreading, or affecting daily life, a quick call and a specialist’s input can make all the difference in protecting your joint health for the long haul.
Personalizing Your Anti-Inflammation Plan
Every joint is unique—and so is your experience with inflammation.
Before jumping to solutions, pause and map out which joints are inflamed, how long symptoms have lingered, and if you have a diagnosis like osteoarthritis or rheumatoid arthritis.
Picture this: You’re keeping a simple log on your phone, noting when your knee swells or when a stiff finger ruins a morning. Those patterns matter.
Mix and Match for Maximum Results
There’s no universal fix—what works for one person might not work for another.
The best approach combines strategies that fit your lifestyle, preferences, and medical history.
Try grouping your action steps:
- For short flares: RICE protocol, over-the-counter creams, brief rest
- For stubborn pain: Structured exercise, guided therapy, topical NSAIDs, movement-friendly routines
- For tracking trends: Symptom logs, food diaries, daily activity records
Feel like you’re troubleshooting software? You kind of are—only the “bugs” are aches and swelling.
Track and Pinpoint Patterns
Busy professionals love data, and your body is no exception. Use a:
- Simple notes app
- Wearable device data
- Spreadsheet that tracks pain scores, food intake, and activity
Review weekly for triggers or improvements.
When you spot that your knee swells after long drives or after pizza night, that’s real insight. Small patterns can reveal big causes.
Collaborate for Better Results
You’re the product owner here. Come to your next appointment with:
- A list of questions (“Does this supplement really work for my type?”)
- An outline of what you’ve tried and how it felt
- Notes on what doesn’t work
Doctors appreciate data-driven patients. The more specific your plan, the more tailored their advice.
Remember: “The most effective anti-inflammation plan is the one that fits your life.” Your job isn’t to do everything at once—it’s to pick, test, and refine the few habits that move the dial for your joints.
With this approach, you’re not just “managing” inflammation—you’re engineering comfort into your daily routine.
Conclusion
You have more control over joint inflammation than you might think—by making a few strong choices today, you can stack the odds in your favor for lasting comfort and mobility.
Empowering yourself with the right knowledge turns inflammation from a daily saboteur into a signal you can respond to—with clarity, not frustration.
Key Takeaways for Rapid Joint Relief:
- Dial down acute flair-ups: React fast with the RICE protocol and topical relief for immediate comfort.
- Upgrade your meals: Fill your plate with omega-3-rich foods and colorful produce to help quiet chronic inflammation.
- Move (smarter): Even ten-minute walks, gentle stretching, or water-based exercise make a measurable impact.
- Track your progress: A simple symptom log or notes app transforms vague aches into actionable data.
- Know your limits: If pain is severe or persistent, reach out to a specialist—it’s a strategic, not surrendering, move.
Ready to take action?
- Pick one anti-inflammatory meal swap for lunch or dinner today.
- Add a brief walk or stretch break to your workday—set a reminder and treat it like a meeting.
- Log your joint symptoms this week, noting patterns or improvements—data beats guesses.
- If something feels off (red, swollen, persistent), schedule a quick check-in with your healthcare provider.
A few smart changes now can mean years of stronger, happier joints ahead.
Your joints don’t need heroics—they just need consistent, informed attention.
Stay curious, stay engaged, and remember: the best anti-inflammatory plan is the one you actually do.
Your movement is your power. Start engineering comfort today—and let every step forward be your proof.