Key Takeaways
Controlling diabetes is less about rigid rules and more about smart, sustainable strategies that fit your unique lifestyle. These key, scannable steps will help you master the fundamentals, leverage new tech, and build habits that stick—without overwhelm.
- Personalize your diabetes plan by tracking your own diagnostic markers and collaborating closely with your care team for data-driven adjustments.
- Prioritize nutrition fundamentals by choosing whole grains, lean proteins, and healthy fats, and practice portion control and meal timing for sustainable glucose management.
- Make movement your daily superpower—even 21 minutes of moderate activity a day can lower your HbA1c and boost your energy.
- Lean into real-time glucose monitoring using CGMs or smart meters to spot trends instantly and take quick, proactive action when needed.
- Match medication to your needs—work with your provider to customize your treatment based on diabetes type, comorbidities, and evolving lifestyle.
- Build a strong support system with education, mental health resources, and peer groups to improve outcomes and prevent burnout.
- Stack healthy habits with habit-forming tools like digital reminders, checklists, and streak apps—tiny shifts drive long-term success.
- Embrace the latest innovations—from AI-powered health coaching to next-gen medications and digital communities, modern tech gives you a powerful edge.
By applying these actionable takeaways, you'll make diabetes management less of a challenge and more of a personalized, empowering routine. Dive into the full article for step-by-step guidance and expert tools you can start using right away!
Introduction
What if you could wield data, smart tech, and a bit of habit-building creativity to take real control of diabetes—without burning out or missing a beat in your busy schedule?
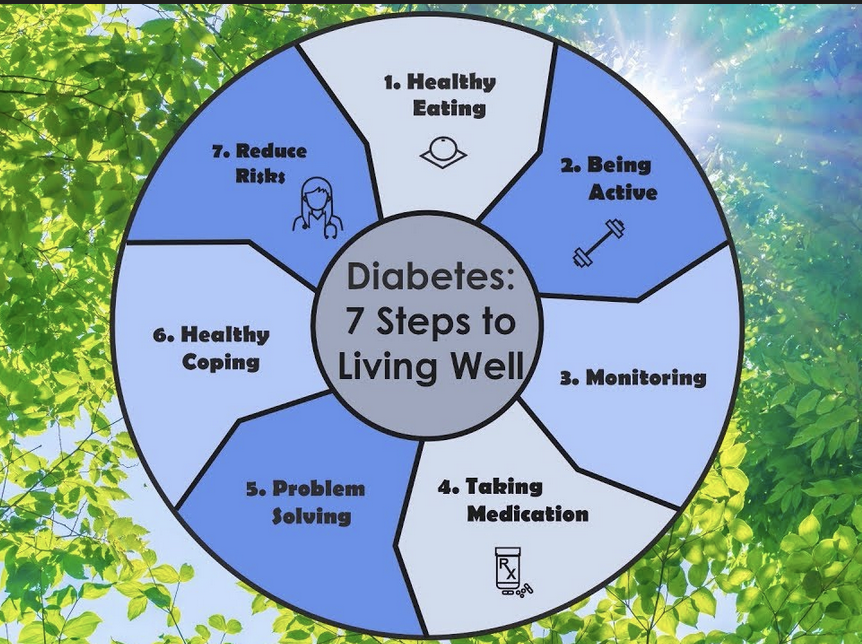
Too often, managing diabetes feels like its own full-time job—one where the rules keep changing and “best” advice gets lost in the noise. But new research shows that putting just 7 core habits on autopilot can help you lower HbA1c, reduce scary complications, and unlock more freedom in your routine.
Think about:
- Sustainable meal hacks (yep, dessert’s still on the table)
- Real-world strategies to work with, not against, your favorite tech
- Personalized plans and smart-monitoring tools that fit your unique workflow
For tech-driven professionals and AI enthusiasts, the landscape is shifting—continuous glucose monitoring, digital health coaching, and even AI-powered meal reminders are turning frustration into actionable insight. No shame, no perfectionism—just progress you can see in your data.
If you’re tired of diabetes being a bottleneck rather than a background process, you’ll learn:
- How to use real-time metrics like HbA1c and “time in range” as your dashboard
- Where to fit in movement—even if you never set foot in a gym
- Ways to sync your work-life chaos with routines that actually stick
By the end, you’ll have a practical game plan powered by science, digital tools, and support systems you can trust—all mapped to your actual lifestyle, not an idealized one.
Ready to create a playbook that puts you (and not your numbers) in the driver's seat? Your customized approach starts with understanding your own unique diabetes profile—so let’s set up your personal baseline.
Top Pick for Blood Sugar Support in 2026
This approach targets the real drivers of unstable blood sugar — not just symptoms.
Most solutions miss this key factor — which is why this one stands out.
Step 1: Understand Your Individual Diabetes Profile
“Think of this step as prepping your playbook—no two diabetes journeys look alike. Personalization isn’t fluff—it’s the most powerful tool you have.”
Are you tackling type 1, type 2, or prediabetes? Each demands a unique approach. The data says it all: what works for your neighbor might do nothing for you. That’s why understanding your own diagnostic markers is step one.
Know Your Numbers and Markers
Keep a close eye on these must-track metrics:
- 𝐄𝐱𝐩𝐞𝐫𝐢𝐞𝐧𝐜𝐞 𝐏𝐫𝐨𝐯𝐞𝐧 𝐀𝐜𝐜𝐮𝐫𝐚𝐜𝐲 𝐰𝐢𝐭𝐡 𝐈𝐌𝐃𝐊 -The IMDK BGM undergoes rigorous...
- 𝐓𝐫𝐮𝐬𝐭 𝐘𝐨𝐮𝐫 𝐈𝐌𝐃𝐊 𝐁𝐆𝐌 - The IMDK Blood Glucose Monitor Kit delivers exceptional accuracy, exceeding international standards....
- 𝐇𝐢𝐠𝐡 𝐒𝐭𝐚𝐛𝐢𝐥𝐢𝐭𝐲 𝐓𝐞𝐬𝐭 𝐒𝐭𝐫𝐢𝐩𝐬 - Advanced 8-Electrode Technology: Reduces interference from common...
- Type of diabetes (type 1, type 2, LADA, MODY, etc.)
- HbA1c (your personal “report card”—aim for ≤6.5% if safe and realistic)
- Glucose trends (fasting, post-meal, overnight dips or surges)
- Comorbidities (heart disease, kidney issues, high blood pressure)
- Family history and genetic risk factors (diabetes can be a team sport—sometimes you inherit your teammates)
Each of these shapes how you and your care team set goals.
Collaborate and Customize Your Plan
Picture this: You’re building your game strategy. Collaborating with your healthcare team is like recruiting expert coaches—endocrinologists, diabetes educators, nutritionists. You’re not expected to do this solo.
Here’s how to make it actionable:
- Bring up patterns: “I’m always low in the afternoon—why?”
- Ask about new tools: “Should I try a CGM or smart meter?”
- Share your work/life setup: “I travel a lot—how do I avoid throwing my routine off?”
Treat your plan as a living document—edit, tweak, adjust with each check-in.
Track, Assess, and Adapt—in Real Time
- ALL-IN-ONE DIABETES LOG BOOK WITH FOOD LIST: More than just a blood sugar tracker – this diabetes log book includes a detailed food list with glycemic index (GI) chart...
- TRACK GLUCOSE, INSULIN, CARBS & MORE DAILY: Stay organized with sections for fasting glucose, before/after meal readings, insulin doses, carb counts, and bedtime blood...
- BUILT-IN MEAL PLANNER FOR WEEKLY SUCCESS: Plan your meals ahead with a simple weekly meal and carb planner to reduce guesswork and stabilize your blood sugar. Great for...
The best teams continually review the playbook.
Use these simple, trackable tools:
- Digital or paper food logs
- Blood sugar diaries (classic, or try an app that syncs with your meter)
- Symptom trackers (energy, mood, sleep—these really matter)
Spotting patterns gets easier with data. Did you know that structured self-monitoring (even just weekly reviews) improves HbA1c and slashes complication risk? One study showed that tailored logs lowered average blood sugar by up to 1% over six months.
Building a personalized diabetes profile helps you respond faster, reduce surprises, and feel more in control—think, “Progress starts with self-knowledge.” Use your personal data as both compass and map. Every trend you track is another tool for smoother, safer days.
⚖️ Know Exactly What You're Eating
Precision matters when tracking carbs. This food scale syncs with apps and makes portion control foolproof.
Check Price →
Step 2: Master the Fundamentals of Nutrition and Eating Patterns
Eating well with diabetes isn’t just about what’s on your plate—it’s about how and when you eat, too.
Picture this: every meal is a chance to dial your glucose where you want it, while still enjoying food you love.
Big evidence alert: intentional weight loss can reduce your diabetes risk by up to 67%—that’s not just a little nudge, it’s a seismic shift.
What Goes On Your Plate—And What Stays Off
Managing diabetes is about maximizing nutrition, not chasing perfection.
🍳 500+ Delicious Diabetic-Friendly Recipes
Stop guessing about meals. This bestselling cookbook includes carb counts, meal plans, and recipes that actually taste good.
[Browse Recipes →]
Here's your at-a-glance hit list:
- Pile on whole grains (oats, barley, brown rice)
- Eat more fruits and vegetables—think color and crunch
- Choose lean proteins (chicken, tofu, fish, beans)
- Aim for healthy fats (avocado, nuts, olive oil)
- Go light on:
- Refined sugars: swap soda for water, pastries for fruit
- Fried foods: savor them occasionally, not habitually
Quotable: “Managing carbs is like budgeting—spend them wisely for better results.”
Portion Control & Timing—Your Secret Levers
It’s not just what you eat, but how much and when.
📦 Portion Control Made Easy: These color-coded containers take the guesswork out of portions. Prep a week of meals in 2 hours.
- 【Sturdy & Reusable】Made of premium thick plastic and strong construction, Dealusy meal prep containers with lids ensure no cracks for your take out meals. They can...
- 【Leakproof & Stackable】: These food prep containers come with tight sealed lids, you can easily stack them and won’t worry that the food would leaks or spills.
- 【Microware Safe & Freezer Safe】: Made of premium food grade plastic, these BPA-free disposable food containers can withstand a temperature from -4℉to 248℉,...
Consider these portion and timing hacks:
- Visual cues: A deck of cards = one serving of meat
- Meal planning: Divide your plate for easy balance—half veggies, quarter protein, quarter grains
- Smart timing: Space meals predictably to avoid peaks and crashes
- “Yes, dessert happens!” The trick? Share that slice of cake, savor small treats, and log it for awareness—not guilt.
Quotable: “Think of meal timing as tuning your metabolism’s clock—consistency pays off.”
Actionable Nutrition Strategies for Busy Schedules
You’ve got deadlines, life, and maybe a sweet tooth. No problem:
🔥 Healthy Cooking Without the Oil
Enjoy “fried” foods without blood sugar spikes. This air fryer makes diabetic cooking delicious and easy.
See It in Action →
- Batch-cook healthy staples on weekends for grab-and-go meals
- Make a grocery list—stick to the perimeter for fresher picks
- Scan restaurant menus for veggie-forward or grilled options (pro tip: “sauce on the side saves surprises”)
- Use a food diary app to spot patterns and micro-wins
Quotable: “The best eating plan is one you’ll actually stick with—ditch the guilt, keep the real-life momentum.”
The real takeaway? Small, mindful choices stack up fast—a few swaps here, a timing tweak there, and your nutrition becomes powerfully sustainable. Make it work for you, not against you.
💊 Natural Blood Sugar Support: Berberine has been shown to lower blood sugar as effectively as metformin in some studies. 1500mg daily dosage. Learn More
Also Recommended: Chromium Picolinate (200-1000mcg) supports insulin sensitivity. Click to Learn More
Step 3: Make Movement Your Secret Weapon
Rethink Exercise: Every Step Counts
Forget the myth that “real” exercise only happens in the gym.
Busy tech pros, marketers, and creatives—movement fits your world wherever you are: at your standing desk, on a quick walk between calls, or dancing in your living room.
Studies show that just 150 minutes a week (about 21 minutes a day) of even moderate activity can lower your HbA1c by up to 0.7%—a major win for long-term diabetes control.
Use this as a permission slip: All movement matters, not just structured workouts.
Exercise Options Built for Your Schedule
💪 Strength Training Anywhere
Build muscle and boost insulin sensitivity with zero gym membership. Includes 5 resistance levels and exercise guide.
Start Today
Picture this: You’re sliding on comfy sneakers, setting a step target on your fitness tracker, and racking up “wins” throughout the day.
Mix and match these movement types for maximum benefit:
- Walking: Easiest to start, lowers blood sugar post-meals
- Strength training: 2-3 times per week helps build muscle and increase insulin sensitivity
- Flexibility/balance: Yoga, stretching, and mobility exercises cut fall risk
- Active fun: Playing with kids, gardening, dog walks, or VR sports—it's all “exercise” on your terms
Your body and your data will thank you for switching things up.
🧘 Low-Impact, High Results
Perfect for flexibility and balance exercises. Extra-thick cushioning protects joints during floor work.
Shop Mats
Smart Ways to Fit Movement Into Your Routine
The best exercise plan? The one you’ll actually do.
Try these habit-building strategies designed for tech-enabled, busy lives:
- Pair activity with tech: Set up reminders, track steps, or schedule “movement meetings”
- Aim for milestones: Celebrate hitting 1,000 more steps, an extra rep, or a new park walked
- Overcome barriers: Bad weather? Try short YouTube routines, resistance bands, or walking in place during video calls
Every small action adds up—“Consistency beats intensity every time.”
Taking Action—Momentum Matters
If motivation tanks or life gets complicated, simply adjust your routine; progress, not perfection, drives results.
Lean into data: Track changes in energy, sleep, and mood as your step count grows.
Recruit a workplace buddy for accountability, or challenge your team to a daily “Micro-Movement” streak.
Here’s your playbook for diabetes control: Move every day, track what counts, and celebrate the wins—big or small. This is how sustainable progress starts now.
Step 4: Embrace Real-Time Monitoring and Glycemic Targets
Knowing your diabetes numbers isn’t just a box to check—it’s the secret weapon for smarter, more confident self-management.
Think of metrics like HbA1c, daily glucose, and “time in range” as your personal performance dashboard. Each number tells a story about what’s working and what needs adjustment.
Zero in on the “Key Numbers” Every Pro Watches
- HbA1c: Target ≤6.5%—if that’s safe for you
- Time in Range: Aim for 70%+ in 70-180 mg/dL using CGM
- Glucose Variability: Keep swings predictable; ≤36% coefficient of variation is a solid goal
When you see your numbers trend off-course, you’re looking at an early-warning radar—not a report card, but an actionable prompt.
“Know your numbers, own your next move.” That’s your rallying cry.
Next-Level Tools Make Monitoring Smart & Sustainable
- Glucose Strips not included
- Glucose Strips needs to be purchased separately.
- Large Easy to read display
💰 Budget-Friendly CGM: FreeStyle Libre 3.
💵 Save on Test Strips Buy in bulk and save 40%. 200-count container.
Similar features to Dexcom at lower cost.
✓ 14-day sensor life (vs Dexcom's 10 days)
✓ Real-time readings
✓ No fingerstick calibration
✓ Often better insurance coverage
Perfect if: You're new to CGMs or want to try before committing to Dexcom.
Gone are the days of finger-stick fatigue. Smart tech is transforming diabetes monitoring into real-time feedback you can actually use.
- Continuous Glucose Monitors (CGM): Show trends minute-by-minute, zap alerts when you're trending high or low
- Connected Meters & Apps: Automatically log, chart, and even predict glucose responses
- Personalized Insights: Some systems now auto-suggest adjustments (like, “Eat before exercise” or “Reduce post-meal carbs”)
Picture this: Glancing at your phone, you spot a glucose spike. Instant notification nudges you to act—grab water, take a walk, or check in with your care team. It’s like having a personalized health coach in your pocket.
Make Real-Time Data Your Decision Engine
Monitoring is more than data collection; it’s about making decisions in the moment.
Every reading creates a feedback loop:
- See a pattern? Adjust tomorrow’s lunch.
- Get an alert? Respond before it becomes a crisis.
- Weekly trends? Review with your clinician to update your plan.
Current best-practice guidelines now urge CGM not just for those on intensive insulin but even for many with type 2 diabetes. Why? CGM use has been shown to improve control in both, helping you spend more days “in range”—not on the glucose rollercoaster.
Here’s the upshot: Track your data, spot patterns, and take quick, low-friction action. Over time, these micro-adjustments stack up, powering both your confidence and your long-term health.
Memorable takeaway: “You don’t have to guess. Every data point puts you in the driver’s seat.” That's progress made visible—one swipe, one decision at a time.
Step 5: Personalize Your Medication and Treatment Plan
Personalizing your diabetes meds isn’t about following a basic template—it’s about matching the right tools to your body and goals.
Think of your medication plan as a custom playlist: what works for one person might be all wrong for the next.
Your prescription should flex as your health—and life—evolves.
🧊 Keep Insulin Safe—Anywhere, Anytime
This medical-grade cooler keeps insulin at perfect temperature for 12+ hours.
✓ TSA-approved for travel
✓ Fits 4-6 insulin pens
✓ Includes ice packs
✓ Compact enough for daily carry
Essential if: You travel, work outside, or store backup insulin in your car.
The Diabetes Medication Lineup: What Fits, and Who Decides?
💡 My #1 Recommended Solution for Blood Sugar Support
Stop Letting Blood Sugar Run the Show. Trusted by thousands and available now with free shipping.
Different diabetes types have different “main acts.”
For Type 2 diabetes, your care team usually starts with:
- Metformin – Most people's starter. Low cost, well-proven.
- GLP-1 Receptor Agonists (GLP-1 RAs) – Great for heart health, often helps with weight loss.
- SGLT2 Inhibitors – Known to protect the kidneys and the heart.
- Insulin – May be needed if blood sugar stays high, especially if A1c is above 9-10% or symptoms are severe.
For Type 1 diabetes:
- Intensive insulin therapy is non-negotiable—think of it as your most critical hardware upgrade.
“Matching your meds to your personal risk factors is how you unlock next-level control—no generic algorithms here.”
The Comorbidity Connection: One Size Doesn’t Fit All
Your other diagnoses can totally shift your diabetes meds game. Here’s how the experts recommend matching:
- Cardiovascular Disease (ASCVD): Prioritize SGLT2 inhibitors and/or GLP-1 RAs
- Heart Failure or CKD (eGFR ≥25): SGLT2 inhibitors rise to the top
- Metabolic Dysfunction-Associated Steatohepatitis (MASH): Pioglitazone, GLP-1 RA, or dual GIP/GLP-1 RA
Plus, statin therapy comes into play for most adults aged 40-75, even without ASCVD, and blood pressure control is just as vital for big-picture protection.
“Personalization is more than comfort—it's how science saves lives.”
Intensifying, Combining, and Managing Meds in Real Life
If your A1c isn’t in the target zone (≤6.5% when safe), or you have complications, your provider might:
- Add on meds (combo therapy)
- Consider injectables or switch up classes
- Factor in side effects, cost, and insurance coverage
Use checklists and pill organizers—miss a dose? Never double up, and always check with your team.
Conversations matter: Ask about lower-cost options, generics, or how new drugs in the pipeline might fit your needs.
“Picture this: Your phone dings, your tracker alerts you, and you’ve got every dose on schedule—diabetes doesn’t outmaneuver you.”
Personalizing your treatment is non-negotiable for beating diabetes at its own game. Knowing your options and building a plan with your care team sets you up for long-term success—on your terms.
💊 Never Miss a Dose Again: Large compartment pill organizer with AM/PM slots for each day. Perfect for multiple medications. Shop Organizers!
Step 6: Build Your Diabetes Support System
📚 Learn from the Best: “Think Like a Pancreas” – The diabetes management bible…
Building a diabetes support system isn’t just nice to have—it’s a proven game-changer for blood sugar control.
Type 2 Diabetes Self-Care and Daily Management Guide: Transform Your Diabetes: 2026 Cutting-Edge Strategies To Better Living, mental health, and real-world results.
Diabetes Self-Management Education and Support (DSMES) can lower HbA1c by an average of 0.5%, slash medical costs, and reduce risky hospitalizations, making every hour invested pay off.
Think of DSMES as your step-by-step playbook for tough moments you didn’t see coming.
What Does a Real Diabetes Support System Look Like?
Let’s break it down into practical components you can start using immediately:
- Skills training: Role-play awkward restaurant orders, work out tricky social situations, or rehearse communicating your needs (“picture this: telling a waiter you need a carb count, without flinching”).
- Family teamwork: Get everyone on board—host mini family meetings, share symptom checklists, split up meal planning and shopping duties.
- Behavioral approaches: Take a page from professional therapy with group classes, online forums, or even text-based peer support to keep motivation alive.
Emotional Support and Mental Health Matter
Managing your numbers is just one part of the story. Coping skills, stress management, and emotional wellness are equally critical for diabetes control.
- Notice signs of burnout or anxiety? It’s smart—not weak—to reach out for mental health support.
- Use visual reminders like notes, calendars, or wellness apps to normalize “checking in” with yourself.
🎾 Quick Stress Relief: Squeeze away anxiety during tough moments.
Make Support Multi-Layered and Ongoing
There’s no single magic bullet—real success comes from stacking multiple types of support:
- Professional guidance: Lean on endocrinologists, diabetes educators, coaches, and case managers.
- Community resources: Join local meet-ups, virtual groups, or dive into platforms like Beyond Type 1’s app for real-time crowdsourced experience.
The research is clear: people who build robust support networks have better numbers and fewer diabetes-related complications. “Your best progress happens when you feel less alone—no matter how tech-savvy you are.”
In a world built on teamwork, assembling your diabetes support crew can be the most transformative step—think of it as your personal pit crew for the road ahead. Start with a single conversation or resource this week, and watch how your confidence—and your health—get a boost.
Step 7: Foster Sustainable Habits for Long-Term Success
Creating habits that stick is the foundation of lasting diabetes control—not just one-off wins. Think of habit formation as “stacking blocks”: you build new routines by attaching them to existing ones, making change less overwhelming and more automatic.
Picture this: tying your blood sugar check to your morning coffee or pairing a healthy snack with your afternoon screen break. Tiny steps, big impact.
Harness Practical Habit-Forming Tools
The healthiest routines thrive on consistency and reminders. Fill your environment with cues that nudge you toward good choices:
- Visual cues: Place your glucometer or medication where you’ll see it
- Digital tools: Use habit-tracking apps like MySugr or Streaks to monitor progress
- Checklists: Keep daily logs for meals, exercise, and meds
- Smart reminders: Automate alerts for blood sugar checks, movement breaks, hydration
Sharable line: “The right reminder at the right time can totally change your day—and your numbers.”
Make Sleep, Mindfulness, and Stress Relief Your Essentials
Don’t sleep on this—literally. Sleep debt increases insulin resistance and derails blood sugar, fast.
- Prioritize sleep: Aim for 7-9 hours as a non-negotiable
- Practice stress reduction: Integrate short mindfulness breaks, deep breaths, or guided meditations
- Track your mood: Use journaling or apps to spot connections between stress and sugar swings
Quotable insight: “Stress management isn’t an extra—it’s a core part of your diabetes toolkit.”
Adapt, Review, and Celebrate Your Progress
Routines should flex with real life. Every 3-6 months, review your action plan with your care team:
- Screen regularly: Schedule checks for your eyes, feet, kidneys, and mouth
- Audit your habits: Are your reminders and routines working—or do they need a tune-up?
- Celebrate wins: Recognize even half-steps forward (“Progress, not perfection!”) with a reward or a shout-out in your support group
Imagine: a calendar filled with green checkmarks, a streak on your app, or sharing a success story with friends—these micro-rewards keep you moving.
When you habit-hack your routine and see results, diabetes management becomes something you do, not just “try.” The key: anchor small actions to your life, track them, and keep adjusting. Consistency plus small celebrations build unstoppable momentum.
Integrating Current Innovations and Trends in Diabetes Control
Staying on top of the latest diabetes breakthroughs isn’t just interesting—it’s essential for staying ahead of your health curve.
Right now, continuous glucose monitoring (CGM) is moving mainstream, not just for insulin users. There’s a wave of new guidelines recommending CGMs for people with type 2 diabetes—even if you’re not on insulin—because the tech gives you real-time glucose numbers and actionable feedback.
Picture this: A busy entrepreneur uses a discreet arm patch CGM synced to their smartphone. Every meal, every workout, every late-night snack instantly shows up on an easy dashboard—no more guesswork, just smart choices.
Emerging Tools: Medications and AI Assistants
Innovation isn’t just about devices.
- New medication classes—like GLP-1 and GIP/GLP-1 combination drugs—are slashing risks for heart, kidney, and liver complications, especially for those with comorbidities.
- AI-powered platforms offer automated health coaching, meal feedback, and symptom alerts—think of your phone doing the heavy lifting on your management plan.
“Personalized medicine is changing the rules—your diabetes plan can now adapt to you, not the other way around.”
Prevention, Digital Coaching, and Early Action
There’s a powerful shift toward catching diabetes earlier.
- Guidelines suggest screening begins at age 35, with risk-focused referrals for intensive lifestyle programs proven to cut type 2 diabetes risk up to 67%.
- Digital coaching apps send reminders, celebrate milestones, and even troubleshoot social or travel scenarios with you—behavioral nudges that actually stick.
The new mindset? “Let’s stop diabetes before it even starts.”
Remote Care and the Rise of Digital Communities
Online care is exploding—virtual visits, digital peer groups, and telehealth check-ins are making expert care more accessible than ever.
- Join an AI-powered community group where members swap real-time glucose tips, recipe hacks, and medication updates.
- Use telehealth for prescription adjustments, symptom reviews, or even quick motivational pep talks.
“Community-driven problem-solving is where real, sustainable change happens.”
What to Watch For in the Next 1-2 Years
The diabetes toolbox keeps expanding:
- Broader CGM access and insurance coverage—even for mild cases
- Cheaper, smarter medication options tailored to your unique needs
- Next-gen habit tracking apps that “coach” you with every tap
If you’re serious about controlling diabetes, now is the time to embrace fresh tools and strategies that fit seamlessly into your workflow.
Ultimately, think of innovation as your “health edge”—use tech and new science not just to track your numbers, but to make them better, every single day.
Practical Tips, Resources, and Expert Tools
The right resources are your secret weapon for mastering diabetes, whether you’re tracking blood sugar or fine-tuning your meal plan.
Stay one step ahead with support from reputable organizations and vetted digital tools—a well-picked toolkit can turn overwhelm into action.
Go-To Websites and Leading Organizations
You want advice that’s science-backed, not guesswork.
Bookmark these trusted sources for up-to-date guidance:
- American Diabetes Association (diabetes.org)
- Centers for Disease Control and Prevention (cdc.gov/diabetes)
- Beyond Type 1
- JDRF (for type 1 diabetes)
These sites break down everything from medication comparisons to CGM tips in clear, jargon-free language.
Smart Apps, Trackers, and Templates
Not all tools are created equal—choose apps that keep it simple and safe.
Top picks for mobile and web:
- MySugr (glucose tracker and reports)
- Carb Manager (meal logging and nutrition info)
- BlueLoop (meds, insulin, and activity logs)
- Glooko (integrates devices for all-in-one monitoring)
Download free templates tailored to diabetes care:
- Daily food and glucose logs
- Weekly meal planners
- Exercise calendars for habit building
- Medication schedules to avoid missed doses
Advanced Learning and Trusted Guidance
Ready to geek out on the “how” behind your numbers or devices? Dig into:
- CGM deep dives (e.g., ADA’s tech webinars)
- Medication comparison charts by trusted nonprofits
- Lifestyle change action plans with real-world strategies
Don’t trust random headlines. Cross-check info with the ADA or CDC—research shows that misinformation can increase risks, so vet every new idea before acting.
Curate Your Own Diabetes Toolkit
Picture this: you test-drive three apps and find one that “just clicks” with your workflow.
Diabetes isn’t one-size-fits-all—rotate tools and templates as your needs (and tech) change.
“If a logbook or app doesn’t stick, let it go. The best tool is the one you’ll actually use.”
The key? Start with one credible resource, layer in digital trackers, and try bite-sized logs or planners that match your energy—small, repeatable wins turn into long-term routines.
Conclusion
Taking control of diabetes is more than a checklist—it’s a proactive, tech-savvy journey that puts you in charge of your health, your data, and your outcomes.
When you leverage smarter monitoring, personalize your strategy, and harness practical support, you transform daily management into real momentum. That’s true empowerment—and it’s doable today.
Here’s what you can implement right now:
- Track your data thoughtfully—use a CGM, glucose log, or app to spot patterns you can act on.
- Dial in nutrition and movement—batch healthy meals, set a daily step target, and pair new habits to routines you already love.
- Collaborate—don’t fly solo; connect regularly with your healthcare team and support networks.
- Harness technology—explore a new diabetes app or community, and automate reminders so your care fits into your life seamlessly.
- Audit & celebrate—review one area you want to improve, set a tiny goal, and share your win with a friend or group for instant reward.
Pick one step from this list to start—with every action, you’re stacking the deck in your favor. Even a tiny shift today creates ripple effects for your energy, focus, and long-term health.
You have more tools—and more control—than ever before.
Let’s make diabetes fit your life, not the other way around. Step up, own your data, and celebrate every win, big or small.
Because when you lead with action, progress isn’t a someday thing—it starts now.
🔥 Limited Stock
Don’t Let Blood Sugar Control Another Day
This highly rated solution is available today with free shipping. Backed by a 60-day money-back guarantee — no risk to try.














