Key Takeaways
Joint pain management in 2026 is about smart choices, tech-forward strategies, and real-world results. Whether you’re tackling day-to-day stiffness or exploring breakthrough treatments, you now have more actionable options than ever—and the right info can turn chronic pain into an addressable challenge, not a career roadblock.
- Personalized, multi-modal plans deliver the best relief—combine medications, targeted injections, and tech-enabled movement therapies to match your specific joint pain profile for optimal, lasting results.
- PRP and advanced gel injections outlast steroid shots, offering 12–24 months of pain relief for knee osteoarthritis and helping many avoid or delay surgery—ask about “shock absorber” options like Arthrosamid for durable, low-downtime comfort.
- Genicular nerve ablation and cryoneurolysis provide surgery-free pain reset, using radiofrequency or freezing to interrupt pain signals, with up to 60% of patients reporting major knee pain reduction and most back to their routines in a day.
- Smart movement, gait retraining, and tech-powered PT are game changers—AI analysis, remote sessions, and wearable feedback enable even tech pros to cut knee pain by 30% or more with real-world, time-saving strategies.
- GLP-1 weight-loss drugs and metabolic care now double as pain treatments, with just 10% weight loss slashing knee pain by up to 50% and easing long-term joint load for those with OA.
- Inflammatory arthritis (like RA) is tamed by safer, targeted meds—biologics, small molecule inhibitors, and up-and-coming immune reset therapies reduce pain and joint damage, often with fewer side effects and more control over activity.
- Emerging regenerative and gene therapies are entering trials fast—new piezoelectric hydrogels, growth-factor injections, and gene-silencers are on the horizon, so stay connected for clinical trial access and future-ready care.
Want the inside edge for your joints? Dive into the full guide to compare treatment pros, cons, and the latest innovations—then build a customized game plan that fits both your work and wellness goals.
Introduction
Your morning’s rolling right along—until that familiar, electrifying jolt of joint pain hijacks your flow. If you’re nodding (or maybe wincing), you’re not alone: over 35% of adults worldwide now report recurring joint pain, and it’s the leading culprit behind missed workdays.
But here’s the real headline: 2026 isn’t just another year of “grin and bear it”. Whether you’re building a campaign, crunching code, or hustling to your next meeting, the treatment landscape has shifted in your favor—aching wrists, locked knees, and sore thumbs are officially on notice.
What’s different this time? Innovation is everywhere. You’re not stuck choosing between ice packs and painkillers. Tech-driven therapies and science-backed routines are reshaping what relief—and even real repair—looks like.
Expect to discover:
- Regenerative options (think PRP, growth factors, and advanced injectables) that go beyond symptom-masking
- Ultra-personalized treatment plans matching your arthritis type, workload, and digital lifestyle
- Cutting-edge tools for movement, remote rehab, and non-drug solutions you can use between Zoom meetings
The big win? You’ll leave knowing how to compare emerging and classic treatments, what works right now (and why), plus how to spot the next breakthrough before it’s mainstream.
If you’re ready to move pain off your daily agenda—and reclaim those friction-free workflows—let’s start by decoding exactly what’s causing joint pain in 2026, and why that’s the key to finally getting ahead of it.
Understanding Joint Pain: The 2026 Landscape
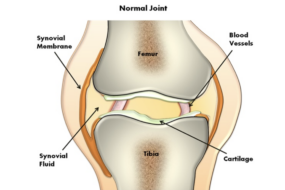
Joint pain isn’t just an “aging problem”—it’s the discomfort, stiffness, or aching you feel where two or more bones meet.
Let’s make it simple: acute joint pain means short-term, often after an injury, while chronic joint pain lasts for months or even years, disrupting daily life.
What Causes Joint Pain in 2026?
You’re probably seeing these pop up in your own world (or among friends and family):
- Osteoarthritis (OA): The most common culprit, caused by cartilage wear-and-tear
- Rheumatoid arthritis (RA): An autoimmune attack on joint linings
- Injury or repetitive use: Sports, job, or tech-life overuse
- Aging: Time brings stiffness—even in ambitious, active pros
People over 50 and anyone with tech-heavy routines often notice joint pain impacting both productivity and quality of life.
The Numbers: Trends and Impact
By 2025, over 35% of adults report recurring joint pain, making it the #1 reason for missed workdays worldwide.
Joint pain can mean:
- Missed project deadlines due to hand or wrist pain
- Fitness goals on hold when knees or hips flare up
- Daily movements limited, from walking meetings to typing speed
“Picture this: you’re prepping a pivotal demo, but your thumb joint locks up, turning every mouse click into a mini-ordeal.”
2026: A Turning Point for Treatment
So, why is this year different? Innovation is rewriting the playbook.
- New treatments like low-dose radiation therapy deliver relief in weeks, not months
- PRP and growth-factor injections aim to actually repair joints, not just dull pain
- Focus has shifted from just surviving pain to preserving and regenerating joint function, targeting the root causes
Expert evidence in 2026 emphasizes:
- Personalized options: Matching therapy to your type of arthritis and daily tech/lifestyle needs
- Multi-modal plans: Combining smart medication, movement innovations, and tech-driven rehab for lasting results
- Regenerative therapies: Future-facing, but some are already speeding recovery and delaying surgery today
What This Means for You
The landscape now lets you choose from more tools than ever—think pain relief with joint protection and even regeneration on the menu.
If you want the sharpest edge, work with your care team to tailor solutions: compare classic and emerging therapies, mix and match approaches, and stay updated as the science (and your joints) keep moving forward.
Medical Treatment Options: Prescription and Over-the-Counter Solutions
When joint pain flares up, fast relief matters—so let’s break down what’s actually working in 2026, from your medicine cabinet to your doctor’s script pad.
For many, over-the-counter (OTC) meds are the first stop:
- Acetaminophen (Tylenol): Go-to for mild pain, gentle on the stomach, but less effective for inflammation.
- NSAIDs (like ibuprofen, naproxen): Tackle both pain and swelling, but watch out for stomach, kidney, or heart risks—especially long-term.
- Topical creams (diclofenac, salicylates): Rub-on relief that targets specific joints (think knees, hands) with fewer whole-body side effects.
“Grab what’s in your cupboard—just don’t ignore label warnings or mix products without guidance!”
If basic options stall out, talk with your doc about prescription medications:
- Stronger NSAIDs: Prescribed versions pack more punch for tough pain, but safety checks are a must.
- COX-2 inhibitors (celecoxib): Engineered for fewer stomach woes, still powerful for arthritis.
- Severe pain solutions: Tramadol is sometimes considered short-term, though most experts steer clear of opioids for chronic joint pain.
Picture this: You’re trying to power through meetings, but your knee’s throbbing—your doctor may suggest you “upgrade” your pain plan with these targeted meds.
Corticosteroids can be a game-changer for short-lived flares:
- Oral pills: Tackles body-wide inflammation—great for a targeted reset but not for routine use.
- Joint injections: Delivers rapid, focused relief (often within days), but overuse can speed cartilage wear.
- 2026 update: Leading guidelines now cap most steroid use at 2–3 times per year per joint, due to cartilage risk.
“Steroid shots work fast, but think of them as a reset button, not a cure.”
For inflammatory arthritis (RA, psoriatic arthritis), innovation keeps coming:
- Targeted oral drugs: New pills zero in on specific inflammatory pathways, offering control with fewer steroids.
- Safer biologics: Updated in 2026, these injectable or infusible meds reduce joint damage with fewer immune side effects, giving you long-term protection and peace of mind.
Comparison At a Glance:
To find your ideal match, ask your doctor:
- “Which option fits my daily routine and medical risks?”
- “Is there a safer switch if I’m worried about side effects?”
- “What’s the long-term plan, and how do we measure progress?”
A quick pharmacist huddle or a candid check-in with your provider can tailor your meds to your joint pain profile, tech-lifestyle, and goals—so you can get back to your real work, not managing symptoms.
When it comes to medications for joint pain, the smartest move is having an informed conversation—your ideal treatment depends as much on what you need as what today’s best evidence supports.
Injection and Biologic Therapies: Innovations for Pain and Regeneration
Platelet-Rich Plasma (PRP) & Growth Factor Injections
PRP injections use your own blood—spun down to concentrate platelets—then injected directly into the painful joint.
Here’s the 2026 update:
- PRP relieves knee osteoarthritis pain for 12–24 months—around double the duration of most steroid shots.
- Trials show PRP works best for mild to moderate OA—it can delay knee replacement and, in some cases, slow cartilage loss seen on imaging.
Growth factor injections are a hot research area. These deliver lab-purified proteins, stimulating tissue repair and directly decreasing inflammation.
You’ll see “picture this” moments: a busy professional walks into a clinic, gets a PRP shot during lunch, and can be back at their standing desk by afternoon—relief that could last a year or more.
Bite-sized takeaway: “For many, PRP means fewer trips to the clinic and longer stretches between flares.”
Hyaluronic Acid and Advanced Gel Injectables
Hyaluronic acid (HA) injections have been a mainstay: they lubricate the joint, reduce friction, and cushion impact.
What’s changed in 2026?
- Recent data: 49% of knee OA patients report “good” to “excellent” pain improvement after HA.
- Arthrosamid—an advanced hydrogel—lasts longer, creating a “soft insert” effect inside the knee joint for lasting comfort.
Who benefits most?
- HA/Arthrosamid: active adults (40–80+) with knee OA wanting to stave off surgery.
- Both picked for minimal downtime—expect a quick office visit and walking out the door 20 minutes later.
Memorable quote: “Think of Arthrosamid as a shock absorber for your joint.”
Corticosteroid Injections: Fast Relief, Important Caveats
Steroid shots act fast—most people feel better in 2–5 days—but relief often fades within 6–12 weeks.
2026 safety updates:
- Repeat use may speed cartilage loss in some.
- Newer guidance: Best for sudden flares—not regular maintenance.
- Compared to PRP or HA, steroids are the “quick fix” but not the long-term solution.
Suitability Matrix:
- Sudden severe pain? Steroid shot.
- Lingering moderate OA? PRP or HA/Arthrosamid.
- Trying to delay knee replacement? Consider PRP or hydrogel.
What to expect:
- Injections are in-office (10–20 min), mild soreness after, minimal downtime.
- Risks: swelling, rare infection, short-term ache.
Each of these therapies is reshaping joint pain treatment, offering options from short bursts of relief to sustained regeneration. The best match depends on your pain pattern, past results, and your timeline—knowing what’s new helps you ask the right questions at your next appointment.
Nerve-Targeting Pain Procedures: Advanced Options for Persistent Joint Pain
What Are Nerve-Targeting Joint Pain Procedures?
Persistent joint pain that lingers despite medications, injections, or physical therapy is a real challenge—especially when it locks you out of activities you love.
Nerve-targeting procedures focus on interrupting pain signals from the joint to your brain, delivering powerful relief without major surgery.
Picture this: Instead of managing pain from the “outside,” these treatments flip the switch right at the source—the nerves responsible for transmitting those relentless pain messages.
Prepare to meet two of 2026's most requested options: Genicular Nerve Ablation (GNA) and Cryoneurolysis.
Genicular Nerve Ablation (GNA): Quick Overview
GNA uses radiofrequency energy delivered by a needle to heat and disrupt tiny nerves around the knee—think of it as hijacking the joint’s pain “WiFi.”
Here’s how it works:
- A local anesthetic numbs the area
- A thin probe targets nerves using imaging guidance
- Gentle heat is applied for just a few minutes
The best part? Most patients resume normal activity within a day.
Average pain relief lasts weeks to months—sometimes up to one year, especially for knee osteoarthritis.
GNA is ideal for:
- Adults with knee pain unresponsive to meds or injections
- Those hoping to avoid or delay surgery
- People seeking a minimally invasive option with proven short-term outcomes
A standout statistic: Up to 60% of patients report significant pain reduction after GNA in recent studies.
Cryoneurolysis: Freezing Away Joint Pain
Cryoneurolysis takes a different tech-forward approach: targeted freezing of nerve endings using a special probe, shutting off pain transmission temporarily.
- The procedure lasts about 20–30 minutes per joint
- There’s minimal downtime—even for active professionals
- Relief typically lasts several months, with quick symptom return if needed
How does it compare to GNA?
- Both are outpatient, image-guided procedures with rapid recovery
- Cryoneurolysis is “cold-based,” while GNA uses heat
- Side effects are mild for both—think numbness or temporary soreness
Cryoneurolysis shines when you want flexibility in repeating treatment or prefer a non-heating approach.
When to Consider Nerve Procedures—and What Are Their Limits?
You might ask, “Should I choose nerve procedures over injections or surgery?”
Consider nerve-targeting interventions when:
- Pain persists after trying medications or biologic injections
- You want to avoid downtime from surgery
- You’re seeking pain relief, not joint repair or regeneration
Key limitations to note:
- These procedures are designed to block pain—not heal or reverse joint damage
- Results vary; repeated treatments may be needed
- They’re typically NOT recommended as first-line for inflammatory arthritis (like RA)
If modern pain management means maximizing your movement and minimizing downtime, nerve-blocking options like GNA and cryoneurolysis could be the practical “reset button” you need. Remember: Ask your doctor about candidacy, expected results, and whether these quick recovery procedures fit your pain profile in 2026.
Non-Drug Approaches: Lifestyle, Movement, and Rehabilitation Strategies
Innovative Physical Therapy and Movement Interventions
Physical therapy isn’t what it used to be. In 2026, PT clinics are blending classic hands-on care with tech-enabled tracking, digital coaching, and remote check-ins—making expert guidance accessible even from your couch.
One major newcomer: gait retraining. Think of it as “reprogramming how you walk” with a physical therapist’s help or even AI analysis. Recent clinical trials show that adjusting your step—changing stride, foot placement, and pressure—can reduce knee pain by 30% or more in people with osteoarthritis.
- Personalized strategies now pair real-time feedback tools (like wearable sensors) with expert tweaks, so you’ll know instantly if you’re protecting your joints.
- Remote PT sessions are quickly catching on for hip and knee pain, letting you get targeted routines, progress check-ins, and adjustments without leaving home.
“Imagine correcting how you move in the time it takes to brew your coffee—PT in 2026 is all about convenience and results.”
Weight Loss and Metabolic Management
Carry extra weight? You’re in good company: Over 60% of knee OA patients are overweight or obese. The big 2025 headline? GLP-1 agonists (think Ozempic®, Wegovy®) and similar meds, originally for diabetes weight loss, are now proven to reduce joint pain by lowering body weight—relieving pressure with every single step.
- Losing just 10% of body weight can cut knee pain scores by up to 50%.
- Modern weight-loss drugs are making these targets more realistic than ever.
Picture this: each pound lost could mean thousands of pounds less stress on your knees each year—a fact that makes every healthy change count.
Mind-Body and Low-Impact Exercise Approaches
Tai chi and similar mind-body programs are quietly dominating the headlines. Latest studies show tai chi improves pain, function, and balance in knee OA—even rivaling some drug therapies.
Want consistency? 2026’s tech tools make building a “movement habit” easier than ever:
- App-based exercise reminders
- Wearable step trackers
- Streaming live group fitness or mobility classes, including adaptive sessions for beginners
- Start with two short sessions per week and build up as you gain confidence.
Pulling Your Plan Together
Combine what works best for you—try gait retraining, add a weight-management strategy, and pick a low-impact exercise program. Use digital appointments and smart reminders to stay on track, all while keeping pain in check.
Key takeaway: Non-drug joint relief in 2026 means smart movement, sustained weight change, and tech-enabled support—not just “more exercise,” but a targeted strategy you can actually stick with, no matter how busy your schedule gets.
Emerging and Regenerative Therapies: The Near-Future of Joint Pain Relief
Next-Gen Injections and Regenerative Gels
Imagine a future where joint pain isn’t just muted—it’s reversed. That’s the promise behind several new therapies now hitting clinical trials and animal studies.
Piezoelectric hydrogel injectables—think of these as “electricity-generating gels.” These materials create tiny electrical charges every time you move, jumpstarting cartilage regrowth. In rabbit studies, a single injection of piezoelectric gel re-formed strong, functional cartilage in roughly 2 months—that’s faster than many traditional approaches even mask pain.
Growth-factor and aging-targeted injectables are also on the horizon. Researchers are using novel proteins and genetic tweaks that literally undo cartilage thinning seen with age. Early mouse studies with “aging-targeted” injections reversed cartilage loss, pointing to a possible anti-aging future for your joints.
“Regenerative injections could mean knee repair, not replacement, is your future choice.”
Gene Therapy and Precision Medicine
Let’s talk about gene-silencing therapy: this technology delivers small RNA molecules—using precision “address tags” that find and shut down the pain and inflammation genes inside your joint. While these treatments are still mostly in lab and animal phases, the potential is huge: imagine one shot turning off pain for months at a time with minimal systemic side effects.
Precision/omics-guided treatments leverage your unique biology. Genome-wide studies have already flagged microRNAs and blood markers that predict who’ll respond best to certain drugs. That means your next treatment could be custom-matched to your joint’s specific needs—precision medicine in action.
“Picture this: a simple blood test tells you the exact treatment plan for your knee or hip pain.”
Stem Cell and Advanced Biomaterial Approaches
Innovation is accelerating with stem cell and advanced biomaterial solutions. These often combine:
- PRP (platelet-rich plasma) or growth factors
- Engineered hydrogels or gene therapy
- Personalized cell or tissue engineering
Clinical trial recruitment is hot—opportunities include pilot studies for hydrogel injections, next-gen stem cells, or gene therapies. The challenge? Availability and unclear long-term effects, but more options enter trials every month.
Wondering what’s accessible now? Most regenerative and gene therapies remain in experimental stages, with enrollment available at university medical centers worldwide.
“If you want in on these therapies, ask your doctor about active clinical trials in your city—new listings appear almost weekly.”
Trailblazing joint pain relief in 2026 means looking beyond painkillers, toward evidence-based regeneration. Track ongoing trials and collaborate with your care team to unlock real, long-term joint health breakthroughs.
Special Focus: Inflammatory Arthritis (RA, Psoriatic, etc.)
Inflammatory arthritis like rheumatoid arthritis (RA) and psoriatic arthritis is different from osteoarthritis (OA)—think “system-wide immune malfunction” rather than just wear and tear.
These conditions bring swelling, stiffness, and long-term joint damage, often starting before age 50 and impacting hands, wrists, or feet.
Latest Treatments Shaping 2026 Care
The treatment spotlight for 2026 is on safer, highly-targeted therapies designed for maximum effect with minimal risk.
Your headline options now include:
- Biologic medications: These lab-engineered antibodies block key immune system signals (such as TNF, IL-6, or IL-17), calming inflammation and often stopping damage cold—cost per dose can range from $1,000-$5,000, but many have biosimilar versions driving costs lower.
- Small-molecule drugs: Oral tablets (think JAK or TYK2 inhibitors) tune down immune overactivity in new, targeted ways; they’re easier to take, work for many who don’t respond to older options, and require regular blood monitoring for safety.
- Cell-free regenerative and tolerance-inducing therapies: Imagine “resetting” your immune system to leave your joints alone—2025 trials are testing antibody infusions and protein-based treatments that retrain immune cells without harsh immune suppression.
How These Treatments Work and Who Should Consider Them
Picture this: It’s Monday morning and your hands are so stiff you can’t type. That’s where these therapies step in—calming the immune storm, protecting joints, and restoring daily function.
Most modern regimens involve:
- Early intervention to slow or stop joint destruction
- Tailored choices based on your genetic, disease, and lifestyle profile
- Ongoing safety checks—especially for infection risk or rare liver/blood complications
You might be a candidate for these therapies if:
- You’ve had joint pain and swelling for weeks or months—not just days
- Standard pain relievers (like NSAIDs) or steroids aren’t enough
- You want not just pain relief but to slow damage and preserve mobility for years ahead
OA vs. Inflammatory Arthritis: Key Approach Differences
Here’s a quick-glance comparison:
Takeaways and What’s Next
Biologics and targeted drugs are rewriting the arthritis playbook—think “less pain, more action, fewer side effects.” If you’re navigating chronic joint swelling or pain, ask your specialist about personalized strategies blending modern meds, monitoring, and possibly clinical trial options.
Your journey is about more than pain relief—it’s about reclaiming movement and control in a busy, tech-powered world.
Choosing the Best Treatment: Decision-Making Framework for 2026
Choosing the right joint pain solution in 2026 is all about matching your profile to smarter, safer interventions—no more “one-pill-fits-all” approaches.
Picture this: You walk into your doctor’s office, X-rays in hand, and leave with a personalized plan that combines medications, advanced injections, and tech-driven lifestyle changes tailored just for you.
Step 1: Assess Your Joint Pain Profile
Kick this process off by mapping out the essentials:
- Location: Is pain in your knee, hip, hands, or shoulder?
- Severity: Mild stiffness or all-day agony? Use a 0–10 pain score.
- Diagnosis: Osteoarthritis, rheumatoid, or another cause?
- Past Treatments: Tried OTC meds, PT, injections, or even surgery?
Each detail changes your top options. For example, hands respond well to low-dose radiation therapy, while knees may benefit from PRP or advanced gel injections.
Step 2: Prioritize Evidence, Safety, and Your Lived Reality
Here’s how to sort through the noise:
- Review what’s proven: PRP can provide relief for up to 24 months (knees), while corticosteroid shots work fast but may wear off in weeks.
- Consider side effects: Weight-loss drugs (GLP-1 agonists) help knees by reducing stress but may not be ideal for every health profile.
- Factor in downtime and access: Genicular nerve ablation offers months of pain relief with a quick recovery—ideal when surgery isn’t on your radar yet.
Step 3: Bring in Specialist (or Not)
Ask yourself:
- Does your pain interfere with major life activities or work?
- Failed standard options (meds, PT)?
- Considering “next-level” interventions (injections, nerve ablation, LDRT)?
If you answer yes, it’s time to consult a specialist for advanced therapies or trials.
Step 4: Build a Personalized, Multi-Modal Plan
Your workflow might look like:
- Start with low-risk basics: PT gait retraining, Tai chi, weight management.
- Add targeted meds/injections: OTC NSAIDs, PRP, HA gel, or novel hydrogels.
- Bring in advanced procedures if needed: Nerve ablation, cryoneurolysis, LDRT.
- Monitor progress with clear benchmarks: Use an app or journal to track pain and function every 2–4 weeks.
Step 5: Ask Key Questions Before You Commit
Arm yourself with this quick checklist:
- What’s the real-world success rate and downtime?
- How do costs and insurance coverage break down in 2026?
- What are the meaningful side effects or risks?
- Am I a candidate for emerging therapies or clinical trials?
- Is there a clear plan for what happens if this doesn’t work?
Remember, “Your best joint pain solution is the one that fits your life, not just your X-ray.”
A little prep and the right questions set you up for the strongest outcomes—a “menu” of options tailored for your work, activity goals, and health realities.
Staying Informed: Trends, Costs, and Access in 2026
What You’ll Pay: Comparing Top Joint Pain Treatments
Joint pain therapies come with a wide price range in 2026, and being prepared helps you budget smartly.
Picture this: You’re choosing between a series of injections or six weeks of targeted physical therapy—what’s the real difference on your wallet?
- Injections (PRP, HA, hydrogels): $600–$2,500 per treatment, depending on type and location.
- Physical Therapy: $80–$180 per session; full programs often total $1,000–$2,500.
- Medications: OTC NSAIDs roughly $15–$30/month; new prescription biologics often exceed $2,000/month.
- Advanced Procedures: Nerve ablation or cryoneurolysis ranges from $2,500–$5,000 per knee.
- Low-dose radiation therapy (where available): $1,500–$4,000 for a full cycle, typically not first-line.
These numbers can shift dramatically based on insurance coverage and local availability.
Insurance Coverage: What’s In, What’s Out in 2026
You’ll want to know up front what your plan covers to avoid surprises.
- Usually covered: Standard physical therapy, initial injections (especially corticosteroids or basic HA), most prescribed medications.
- Frequently out-of-pocket: PRP, newer gels like Arthrosamid, advanced biologics, nerve procedures, and low-dose radiation for OA, unless part of a clinical trial.
- Emerging trend: More plans require pre-authorization or “failed other therapies” before green-lighting advanced treatments.
“It pays to call your insurer in advance and ask detailed questions—don’t assume coverage means zero out-of-pocket.”
Finding and Accessing Cutting-Edge Care in 2026
Locating experts and trustworthy information is no longer optional—it’s strategy.
Here’s how tech-savvy patients are staying ahead:
- Use professional societies’ directories to find board-certified specialists in OA, pain, or rheumatology.
- Check for active clinical trials in databases like ClinicalTrials.gov; local academic centers often have exclusive access to emerging therapies.
- Join reputable patient communities or networks (like Arthritis Foundation programs or digital forums for OA/RA) for peer insight.
- Schedule telemedicine consults with top experts, even out of state—many review your history and recommend targeted local options.
“Ask your specialist: What’s the newest evidence-based option for my profile, and how can I access it?”
Staying On Top of What’s Next
Joint pain care is changing quickly—blink and you’ll miss something new.
Latest research is now shared faster via:
- Subscribed research digests (from NEJM, JAMA, or targeted pain/arthritis journals)
- Webinars and digital summits featuring clinical trial updates and treatment reviews
- Following reputable social media accounts (doctors, hospitals, specialty orgs) for real-time discoveries
Imagine a scenario where you spot a promising hydrogel or gene therapy in early trials… you can now track its progress, join waitlists, and even apply for local studies in one click.
The real edge? Stay curious, ask questions, and never accept “that’s all we have” as your final answer.
Savvy patients in 2026 are connected, informed, and ready to partner in decision-making—keep these strategies close and you’ll have the latest in relief, access, and options at your fingertips.
Conclusion
Personalized, cutting-edge joint pain relief isn’t a distant promise—it’s the new standard for 2026. With smarter therapies, regenerative breakthroughs, and tech-driven rehab at your fingertips, you have more control than ever before.
Your advantage? Mixing medical and lifestyle strategies that match your unique needs—so you can stay sharp, mobile, and fully engaged in both work and life.
Key Takeaways
- Explore combination solutions: Don’t settle; pair medical treatments (like PRP or targeted meds) with smart movement and digital coaching for lasting relief.
- Be proactive with your healthcare team—ask about new therapies, safety, and what fits your real-life workflow.
- Leverage tech: Use apps or wearable trackers to measure progress and keep your plan on track—no missed steps, literally.
- Stay curious: Monitor clinical trials and new strategies—today’s breakthroughs could be tomorrow’s routine care.
Next Steps
- Book a conversation with your provider to review your current plan and discuss newly available options that match your pain profile.
- Identify one digital or lifestyle tool (like remote PT, a step tracker, or a research digest) that can support your daily progress.
- Network with specialists or join patient communities—fresh solutions often come from unexpected sources.
Bold possibilities now outnumber old limits—the only “wrong” move is standing still. Empower yourself to experiment, ask tough questions, and demand the best from modern joint pain care.
Your next step could be the one that brings real relief and new energy to everything you do—so why wait?