Key Takeaways
Diabetes complications can feel overwhelming, but with the right strategies, you can dramatically reduce your risk and protect your quality of life. Here’s what you need to know—distilled for quick scanning and immediate action:
- Act early to prevent complications by keeping your blood sugar in target range—even a single percentage point drop in A1c can slash microvascular risks by up to 40%.
- Watch for acute emergencies like DKA and HHS; sudden symptoms such as nausea, confusion, or rapid breathing demand urgent ER attention—minutes count in these scenarios.
- Screen regularly for “silent” chronic issues by scheduling annual eye, kidney, and foot checks; early detection is your best tool to dodge vision loss or kidney failure.
- Adopt smart lifestyle habits—focus on balanced meals, 150+ minutes of weekly activity, and 7-8 hours of sleep to build everyday resilience against both short- and long-term complications.
- Leverage health technology with apps, smart devices, or CGMs that let you track, analyze, and share your trends—turning data into proactive care and early intervention.
- Build your diabetes support squad by connecting with DSME programs, digital communities, and multidisciplinary teams to tackle challenges and stay motivated.
- Personalize your action plan with a mix of medications, updated therapies, and preventive care—the right routine fits your evolving needs and amplifies results.
- Stay future-focused with innovations like AI-driven risk alerts, remote monitoring, and digital therapeutics—the latest tools are making diabetes management more predictive, efficient, and individualized than ever.
Diabetes may bring extra hurdles, but the right knowledge puts you in the driver’s seat—dive into the full article for practical steps to turn these insights into daily wins.
Introduction
Ever wondered why a single percentage point drop in your A1c can slash your risk of certain diabetes complications by up to 40%? That’s not just a number—it’s your daily choices shaping your future.
If you’re managing diabetes, you already know the drill with blood sugar checks and doctor visits. But what’s not as obvious are the silent complications that can sneak up and impact everything from your next brainstorming session to your weekend plans.
Here’s the truth: 1 in 3 people with diabetes will face some level of kidney damage during their lifetime. Still, with practical know-how and a few smart tweaks, you have the power to tip the odds in your favor.
Whether you’re a tech enthusiast tracking every metric, or a busy pro looking for efficient, actionable strategies, this guide breaks down:
- Why certain complications develop—and the hidden risk factors you can control
- Immediate red flags that signal an urgent problem (plus simple “checklist” habits to recognize emergencies ASAP)
- Long-term protection strategies—from smart screenings and health tech to team-based solutions that keep life on track
- New innovations that are empowering people with diabetes to get ahead of complications using digital tools and AI insights
Managing diabetes doesn’t have to mean waiting for problems to show up. It’s about treating each complication as a challenge you’re absolutely equipped to handle—with the right habits, the right support, and just enough cutting-edge tech to keep you proactive, not reactive.
Ready for a real-world look at the big picture—plus the step-by-step moves that separate “worry” from “winning”?
Let’s start by mapping out exactly what diabetes complications are, why they matter, and how you can spot the earliest signs before they ever slow you down.
Understanding Diabetes Complications: The Big Picture
Living with diabetes isn’t just about daily blood sugar checks—it’s about managing the risk of serious complications that can impact nearly every part of your life.
Picture this: complications are the unexpected “side quests” in your diabetes journey—tricky, but absolutely manageable with the right knowledge and habits.
Why Complications Matter
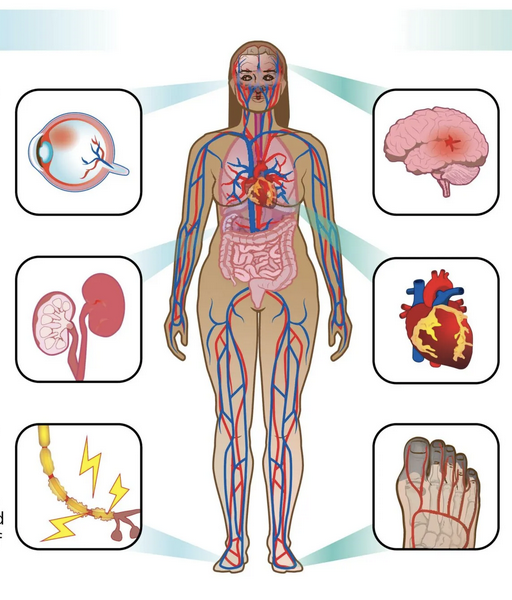
Complications are health problems directly caused by uncontrolled blood glucose over time. They can slowly affect your nerves, kidneys, eyes, heart, and more.
Even with modern tech, diabetes complications remain the biggest threat to long-term health and independence. Almost 1 in 3 people with diabetes will develop some degree of kidney damage in their lifetime. That’s why proactivity isn’t optional—it’s essential.
Acute vs. Chronic: The Two Main Types
Complications fall into two broad buckets:
- Acute complications: Develop rapidly and need immediate attention (think: diabetic ketoacidosis, or DKA, and hyperosmolar hyperglycemic state, HHS).
- Chronic complications: Develop slowly over years and are divided into:
- Microvascular: Small vessel damage (neuropathy, nephropathy, retinopathy).
- Macrovascular: Large vessel disease (heart attack, stroke, peripheral artery disease).
Think of acute issues as sudden storms—visible and urgent—while chronic complications are more like erosion happening beneath the surface, often unnoticed until damage is done.
How High Blood Sugar Drives Risk
Every day spent with high blood sugars increases your risk for both acute and chronic problems. This isn’t just theory—it’s what drives:
- Nerve pain and numbness in your feet (“stocking-glove” pattern)
- Vision loss or blindness (with diabetes the leading cause in adults under 65)
- Kidney failure, dialysis, or transplant
- Heart attacks and strokes—often earlier and more severe than in non-diabetics
“Every percentage point drop in A1c can lower your risk of microvascular complications by up to 40%.” (That’s not just good news—it’s fuel for action.)
Data That Hits Home
Here’s the reality check:
- About 1 in 3 people with diabetes will face kidney disease.
- Diabetes causes over 60% of all non-traumatic lower limb amputations in the US.
- Cardiovascular disease is up to four times more likely for adults with diabetes.
- Many complications develop silently—regular screening is your best bet for catching them early.
Key Moves to Remember
If you only remember three things:
- Keep blood sugar in your target range as much as possible.
- Schedule and actually use your annual screenings—for eyes, kidneys, and feet.
- Treat complications as manageable challenges, not inevitable outcomes. Your routines, not genetics, steer most of your risk.
Diabetes complications may sound daunting, but with informed, consistent actions, you can stay in control and protect your quality of life—every day and for the long haul.
Acute Complications: Urgency in Diabetes Care
Diabetic Ketoacidosis (DKA): Recognize and Respond
DKA is what happens when your body runs out of insulin and starts breaking down fat at high speed.
This triggers a buildup of dangerous acids called ketones—think, “emergency mode,” not business as usual.
Common triggers include:
- Missed insulin doses
- Infections (like the flu or a UTI)
- Severe illness or stress
You’ll spot DKA by symptoms such as:
- Nausea and vomiting
- Fruity-smelling breath
- Deep breathing or confusion
- Rapid heartbeat, abdominal pain
If these symptoms hit, don’t wait—head to the ER. DKA can escalate in just hours and is life-threatening without rapid treatment.
Quotable moment: “With DKA, minutes count. If you’re not sure, act fast—not sorry.”
Hyperosmolar Hyperglycemic State (HHS): The Sneaky Crisis
HHS is a different beast, mostly hitting people with type 2 diabetes and often those over age 60.
It features:
- Sky-high blood sugars (600 mg/dL and up)
- Severe dehydration
- Symptoms building slowly over days to weeks
Look for:
- Lethargy, weakness, or fainting
- Confusion, trouble speaking, or blurry vision
- Dry mouth and extreme thirst
- No major ketone smell
The kicker? HHS has a higher mortality rate than DKA—up to 20%. It’s often missed until someone lands in the hospital very ill.
“Think of HHS as the ‘silent alarm’ of diabetes emergencies—the warning signs can be easy to miss, but the outcome is just as urgent.”
Stay Ahead: Spotting and Managing Emergencies
You can dramatically reduce risk by treating your daily habits like a “diabetes first aid manual.”
Checkpoints you can use:
- Monitor blood glucose frequently, especially when sick (“sick day rules” matter!)
- Know your typical symptoms—and train close friends or coworkers to notice mood changes or confusion
- Keep an action plan handy: Write out when to call your healthcare provider versus head to the ER.
3-2-1 rule: If you’ve vomited 3 times, have 2 sustained high glucose readings, or 1 sign of confusion—seek urgent help.
“Picture this: you, confidently recognizing red flags, calling the shots on what’s an emergency before it becomes one.”
The best way to dodge DKA or HHS: Monitor closely, act quickly, and never go it alone when you’re unsure. Emergencies don’t wait—your plan shouldn’t either.
Chronic Microvascular Complications: Small Vessels, Big Impact
Diabetic Neuropathy: When Nerves Take the Hit
High blood sugar quietly targets your nerves over time, causing diabetic neuropathy—one of the most common diabetes complications.
You might notice:
- Numbness and tingling in your feet or hands (that “stocking-glove” feeling)
- Burning or shooting pain that makes walking or even light touch uncomfortable
- Weakness or loss of balance
Think of this as faulty wiring in your body’s electrical system—the longer wires go unchecked, the greater the risk of foot ulcers, infections, or even Charcot arthropathy (severe joint damage).
“Missing the early warning signals can turn a small issue into a big deal fast.”
Diabetic Nephropathy (Kidney Disease): Protecting Your Filters
Over time, high blood glucose can wear down your kidneys’ delicate blood vessels.
The stats are real: about 1 in 3 people with diabetes ends up with some level of kidney disease.
Without action, the next steps could be:
- Dialysis (regular blood filtering at a clinic)
- Kidney failure needing a transplant
Annual urine or protein tests are your early alarm—catching issues before you ever feel sick. “A simple lab slip today could save you a thousand hours in a dialysis chair.”
Diabetic Retinopathy: Seeing Eye-to-Eye With Risk
Diabetes is now the top reason people under 65 lose their eyesight.
Unmanaged blood sugars damage the tiny vessels that feed your retinas, leading to:
- Blurred or spotty vision
- Loss of sight
- Higher rates of glaucoma and cataracts
Regular eye screenings pull your risk out of stealth mode—most with retinopathy feel nothing until their sight fades. Picture yourself breezing through an eye exam today; that’s your best defense.
Integrated Microvascular Management: Don’t Wait for a Symptom Surprise Party
Here’s the kicker: these complications often develop quietly and painlessly.
If you want to lower your risks:
- Aim for steady glucose and blood pressure
- Schedule annual checks for your eyes, kidneys, and feet—non-negotiable
- Level up your lifestyle (more movement, less stress, fiber-rich meals)
“Screenings and smart habits are your backstage pass to a longer, healthier future.”
Even if you feel fine, staying ahead of microvascular trouble means dialing in your data, routines, and daily choices—before symptoms ever show up.
Chronic Macrovascular and Other Systemic Complications
Cardiovascular Disease in Diabetes
If you have diabetes, your risk for heart attack and stroke doubles compared to someone without it.
That’s because high blood sugar, elevated blood pressure, and cholesterol can all damage your blood vessels—creating a triple threat.
Watch for warning signs like:
- Chest pain
- Shortness of breath
- Sudden weakness or numbness, especially on one side
These can happen even in people under 40.
Cardiovascular disease is the #1 reason for hospitalization in diabetics, driving most long-term disability and early death.
Picture this: going from regular energy to chest discomfort in the middle of a work call—that’s how sudden a complication could appear.
Peripheral Artery Disease & Diabetic Foot Problems
Combine neuropathy (nerve damage) and poor leg circulation, and you have what doctors call “the perfect storm” for foot issues.
Common complications include:
- Foot ulcers: slow-healing sores that can open the door to infections
- Infections: bacteria love elevated glucose
- Amputations: over half of non-traumatic lower limb amputations worldwide happen in people with diabetes
Daily foot checks and protective footwear act like your first line of defense.
A simple habit, like examining your feet every night, could be the difference between early intervention and major surgery.
Beyond the Obvious: Other Complications
Diabetes isn’t just about blood sugar—it can impact nearly every system.
Additional risks include:
- Slowed wound healing, frequent skin infections
- Gum disease (periodontitis) and mouth ulcers
- Carpal tunnel, frozen shoulder
- Osteoporosis (weakened bones)
- Immune suppression
- Rare but serious issues: liver and gallbladder disease
A cut that lingers, or stiff joints that limit your morning routine, might trace back to blood sugar control.
Patterns, Prevalence & Progression
Roughly 1 in 3 people with diabetes will develop serious foot, eye, or kidney complications at some point.
Your risk climbs with:
- Longer duration of diabetes (over 10 years is a major inflection point)
- Poor blood pressure or cholesterol control
- A family history of vascular disease
Spotting early signs and sticking with preventive care can dramatically reduce complication rates.
Key takeaway: Chronic complications of diabetes are common—but they’re not inevitable. Staying alert, proactive, and making small daily checks can protect not just your feet or heart, but your quality of life long-term. One minute of prevention might save you months of recovery.
Strategies for Minimizing and Managing Diabetes Complications
Lifestyle Modifications: The Foundation
Lifestyle changes are your best first defense against diabetes complications.
- Nutrition: Build your meals around a balanced plate—fill half with low-glycemic, high-fiber veggies, add lean proteins, and keep carbs manageable (think brown rice, quinoa, beans).
- Movement: Aim for at least 150 minutes per week of moderate exercise. Brisk walks, dancing, or gym sessions all count—choose something you’ll actually enjoy and stick with.
- Sleep/Stress: Prioritize 7-8 hours of quality sleep and make stress reduction non-negotiable—meditation apps, yoga, or simply stepping away from your screen help lower risk.
- Progress Over Perfection: A minor improvement in routine today beats a perfect plan you never follow.
Picture this: Swapping a nightly TV binge for a post-dinner stroll can make a measurable difference in insulin sensitivity.
“Small changes add up—your daily choices build the foundation for long-term protection.”
Monitoring & Screening: Staying Proactive
Staying in front of complications means anticipating issues before they snowball.
- Self-monitoring: Use SMBG or a CGM system—CGMs give real-time trends, while SMBGs offer point-in-time checks.
- Annual Screenings: Schedule regular tests for your eyes, kidneys, and feet. Log these on your calendar like any priority business meeting—because they are.
- Health Tech: Take advantage of apps and smart devices to track your numbers, spot patterns, and share data with your care team.
One quick fact: Early screening catches issues before symptoms even appear—routine kidney tests can prevent progression to dialysis.
“If it’s not on your calendar, it probably isn’t happening—treat screenings as non-negotiable.”
Medications and Insulin Management
Your treatment plan isn’t one-size-fits-all.
- Follow Regimens: Stick closely to prescribed oral meds, injectables, or insulin pumps for consistent control.
- Stay Flexible: Your needs will change—your provider can help adjust doses, upgrade devices, or try innovative new drug classes as needed.
- New Options: Watch for advances in GLP-1 agonists or automated insulin delivery for safer, more tailored therapy.
Numbers tell the story: Keeping A1c in target range can reduce complication risk by up to 76%.
Education, Support & Empowerment
Mastering diabetes self-management isn’t just about what you do—it’s about what you know.
- DSME Programs: Get expert coaching on everything from carb counting to problem-solving sick days.
- Support Networks: Connect with support groups or digital communities; lean on mental health pros if stress or burnout hit.
- Adapting to Life: Having a plan for travel or unexpected changes makes all the difference.
“Think of your diabetes educator as your custom support hotline.”
Preventive and Routine Care
Preventive care multiplies your protection.
- Don’t skip: Immunizations (flu, pneumococcal, hep B), blood pressure checks, and cholesterol reviews.
- Daily Habits: Perform regular foot self-exams and brush up on oral health to address hidden risks before they become problems.
- Quit Smoking: Halving amputation risk starts by putting out that last cigarette.
“Making foot checks and vaccines a habit now can save you from bigger worries later.”
Personalized & Team-Based Approaches
Personalization turns generic advice into your action plan.
- Create a Care Team: Your endocrinologist, diabetes educator, nutritionist, podiatrist, and pharmacist all bring something vital to the table.
- Know When to Escalate: New or worsening symptoms? Don’t guess—ask.
- Embrace Individualization: The right approach matches your goals, habits, and evolving needs.
Big takeaway: The most effective strategy is the one that works for your real life—make care personal, not just prescriptive.
Every step you take—whether it’s adjusting dinner habits, prioritizing sleep, or setting those annual screenings—directly chips away at the risk of serious complications. Your choices today truly are tomorrow’s protection.
The Future of Complication Management in Diabetes
New Technologies and Innovations
Picture this: Checking your blood sugar isn’t just fingersticks—continuous glucose monitors (CGMs) now stream real-time updates to your phone, alerting you before things go sideways.
Remote monitoring lets care teams see trends and intervene fast, even before a clinic appointment is on your radar.
Digital therapeutics—think highly personalized apps—are rolling out features like:
- Automated lifestyle coaching
- Reminders for meds and sensors
- Data-driven predictions of risk
AI and predictive analytics are changing the game. Algorithms can now:
- Flag users at high risk for kidney or eye issues before symptoms appear
- Help you and your doctor personalize screening schedules
Expect to see organ regeneration studies and new drug classes aiming to actually slow, or even reverse, complications—a serious leap forward, though still in research.
“Prevention is moving from art to algorithm—AI is shrinking the gap between possibility and reality.”
“CGMs and remote monitoring are turning daily diabetes management from reactive to proactive.”
Getting Ahead: What’s Next for Patient-Centered Care
The trend is clear: proactive, preventive, and data-driven care is quickly replacing one-size-fits-all diabetes plans.
Telehealth is more than a pandemic trend—virtual care and e-visits now let you connect with top endocrinologists and educators from anywhere.
Smart health platforms can sync your CGM, labs, and other data, flagging problems early—like a dashboard for your diabetes life.
We’re also seeing a surge in efforts to reduce health disparities. Lower-cost sensors and AI-powered virtual clinics are aiming to reach underserved communities.
“Your diabetes team might soon live in your pocket.”
“Data is powerful—but access, affordability, and equity will decide who benefits most.”
Making It Real: What You Can Do
- Ask your provider about digital tools or CGMs you might be eligible for
- Try out diabetes-focused apps—many let you track, analyze, and share trends
- Watch for research updates, especially if you have long-term complications
Diabetes complication management is becoming smarter, faster, and more individualized—with new tools putting you and your care team one step ahead of risk, not behind.
Conclusion
Managing diabetes complications is about reclaiming control—not just reacting to problems, but steering your health with knowledge, consistency, and the power of today’s technology.
You have more tools and strategies at your fingertips than ever before. Every daily choice, screening, and tech upgrade is a building block for a longer, healthier life—one you can shape on your own terms.
Here’s what you can put into action now:
- Prioritize regular screenings for your eyes, kidneys, and feet—add them to your calendar like any essential business deadline.
- Build consistent routines for tracking your blood sugar and reviewing trends—consider integrating a CGM or smart health app.
- Make small, sustainable lifestyle shifts: add movement to your week, swap in high-fiber foods, and lock in your sleep schedule.
- Connect with your care team—and don’t hesitate to ask about the latest innovations or personalized treatment options.
- Strengthen your support network, both online and off, to stay informed and empowered every step of the way.
Ready to take the next step?
- Audit your current diabetes care habits and pick one area—screenings, routines, or support—to level up this week.
- Try a new app or device to make self-management more engaging and data-driven.
- Share your commitment with a friend or community—accountability turns intention into action.
- Reach out to your provider about upgrading your technology toolkit or therapy plan for more effective risk management.
- Keep an eye out for research and tech updates that could further personalize your approach.
The path to complication-free diabetes isn’t about perfection; it’s about consistent, proactive moves—each one a signal to your future self that you’re fully invested in your health, your independence, and your possibilities.
You are not defined by your risks—but by the actions and habits you choose, starting right now. Take ownership, lean into the new tools available, and stay connected to your goals. Every day offers a fresh chance to outsmart risk and build a healthier tomorrow—one step, one choice at a time.