Key Takeaways
Managing diabetes means giving your skin the same attention you’d give your favorite device—targeted, proactive care that prevents breakdowns before they start. Here are the top actionable skin care strategies for staying healthy, comfortable, and ahead of complications, even on your busiest days.
- Consistent daily skin care slashes risk—small habits like moisturizing and quick daily checks can cut diabetes-related skin issues by up to 50%, keeping infections and dryness at bay.
- Dry, cracked, or itchy skin is an early warning—address these signs with a thick, fragrance-free moisturizer after bathing, and never skip vulnerable spots like feet and legs.
- Gentle cleansing routines protect your barrier—opt for lukewarm water and mild, fragrance-free cleansers, avoiding harsh soaps and hot showers to preserve essential skin oils.
- Foot checks prevent major problems—daily inspection for blisters, calluses, and color changes can help catch concerns before they escalate; always report non-healing wounds or infections to your doctor right away.
- Adapt your routine to the season—use a humidifier in dry months, wear protective gear in cold or windy weather, and apply SPF 30+ sunscreen year-round to bolster defense against environmental stressors.
- Smart product selection matters—pick formulas with ceramides or urea, avoid strong scents, and always patch-test new products to lower your risk of skin reactions.
- Tight blood sugar control shows on your skin—steady glucose levels reduce complications by up to 40%, making hydration, balanced nutrition, and daily movement your skin’s best friends.
- Know when to call for backup—seek help quickly for spreading redness, infection signs, or stubborn wounds; don’t wait for small issues to spiral, as prompt care means easier fixes and fewer long-term setbacks.
With these habits in your toolkit, you can keep your skin strong, comfortable, and ready to match your drive—dive into the full article for step-by-step guides and more smart diabetes skin care tips.
Introduction
Ever notice how a tiny skin crack seems to take forever to heal—or turns into something much bigger—when you’re managing diabetes? You’re not imagining it: up to 1 in 3 people with diabetes experience a skin issue every year. That’s not just a stat, it’s a wake-up call for anyone balancing blood glucose with the rest of life’s daily puzzles.
If you’re a tech-savvy professional who thinks in terms of system health and efficiency, here’s the real-world translation: your skin is an interface, not just a protective layer. Just like ignoring an app update leaves you vulnerable to glitches, overlooking daily skin care with diabetes can slow you down—sometimes with costly results.
The good news? Small, consistent tweaks to your skin care routine can:
- Cut your risk of infections and complications by up to 50%
- Help you spot minor issues before they spiral
- Keep your skin resilient and ready for anything—from marathon coding sprints to weekend hikes
You’ll get practical, zero-fluff strategies you can fit into any workflow, plus a clear breakdown of:
- How diabetes really impacts your skin (spoiler: it’s more than just dryness)
- The most common warning signs and foot care musts
- Daily and advanced skin protection hacks, tailored for busy schedules
- When to tackle issues yourself—and when to ping a pro for backup
Think of this as your skin-safety playbook, grounded in real expertise and built for readers who like their advice as actionable as it is evidence-based.
Ready to rethink your approach? Let’s start by unlocking the core link between diabetes and skin health—and why it deserves a top spot on your self-care checklist.
Understanding the Link Between Diabetes and Skin Health
Living with diabetes means your skin needs extra attention—sometimes even more than your devices or work setup.
If you’ve ever wondered why people with diabetes are so often talking about dry skin or infections, here’s the gist: high blood sugar changes the way your skin works at a cellular level.
Think of your skin as your body’s firewall. When blood sugar runs high for too long, it makes your skin barrier more porous—sort of like leaving your front door cracked open during a dust storm.
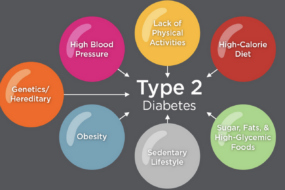
How Diabetes Affects Your Skin
Diabetes disrupts skin health in several key ways:
- Pulls moisture out of the skin, making it prone to dryness and cracks
- Slows down wound healing, so small cuts or scrapes can drag on for weeks
- Weakens immune defenses, raising your risk for bacterial or fungal infections
It’s not just about comfort—these shifts can make a seemingly minor blister or rash spiral into a major problem.
What Does This Look Like in Real Life?
Picture this: You notice a small, cracked patch on your heel. In someone without diabetes, that’s usually no big deal.
But with diabetes, even tiny openings can let bacteria in and kick off infections like cellulitis or serious foot ulcers.
Watch out for common issues like:
- Dryness and persistent itching
- Rashes or areas of flaky skin
- Fungal infections in warm areas (think: between your toes)
- Slow-to-heal wounds, especially on your legs or feet
- Red, swollen, or warm patches that signal possible infection
Why Proactive Skin Care is a Diabetes Power Move
Here’s the shareable takeaway: Proactive daily skin care can slash your risk of complications and infections by up to 50% (based on American Diabetes Association guidelines).
We’re not talking spa days, but consistent small actions—moisturizing, inspecting, and managing blood sugar—pay off big.
If you start thinking about your skin like a real-world interface that needs secure updates and maintenance, it’s a lot easier to prioritize these daily steps.
Staying ahead of dry patches and slow-healing wounds is how you avoid costly issues—and keep your skin as healthy as your next big idea.
Common Skin Issues in Diabetes: What to Watch For
Living with diabetes means your skin often needs extra attention. High blood sugar can quietly set the stage for new skin problems—sometimes long before you notice anything’s wrong.
Think of your skin like a security system: diabetes makes it easier for small issues—like dryness or blisters—to become big problems if they go unnoticed.
Most Common Skin Issues in Diabetes
Here’s what tops the list of skin concerns for people with diabetes:
- Dryness and itching: Caused by dehydration or fluctuating blood glucose levels.
- Rashes: Can stem from dryness, allergic reactions, or yeast overgrowth.
- Fungal and bacterial infections: Especially in skin folds, under breasts, or between toes.
- Slow-healing wounds: Even a minor scrape can linger for weeks due to poor circulation.
A 2023 report found up to 1 in 3 people with diabetes will experience a skin issue each year—so you’re definitely not alone.
Don’t Forget the Feet: High-Risk Warning Signs
Picture this: You take off your shoes and notice a blister, callus, or redness on your foot. With diabetes, these can be more than routine annoyances—they’re red flags that need your attention.
Watch for:
- Ulcers (open sores): May look small, but can hide deeper damage.
- Calluses and thickened skin: Signal repeated pressure or friction.
- Blisters: Pose infection risks, especially if you don’t feel them due to nerve changes.
- Numbness or tingling: Signs of diabetic neuropathy, which make injuries easy to miss.
What’s Okay to Monitor vs. When to Act—Fast
Spot something unusual? Here’s a quick guide:
- Monitor at home if you have: mild dryness, minor itching, or a small callus.
- See a healthcare provider immediately for:
- Spreading redness, warmth, or pain
- Sores that won’t heal after a few days
- Yellow or green discharge (infection alert!)
- Sudden swelling, especially in the feet
Even something as simple as a persistent itch or slow-healing hangnail can snowball if ignored. Early action saves you far more time (and stress) later.
Regular checks and quick responses can keep your skin healthy—and you ahead of surprises. Pay close attention to your skin, especially your feet, and act early when you spot changes. That’s not just smart diabetes care—it’s powerful prevention.
Essential Daily Skin Care Practices
Picture this: small, daily steps that seriously lower your risk of infection, itch, or persistent dryness—even if you’re juggling a jam-packed schedule. When you have diabetes, a skin care routine isn’t just nice to have; it’s as essential as your morning coffee.
Moisturizing: Your First Line of Defense
Moisturize right after bathing—it locks in hydration and fights the dryness that comes with fluctuating blood sugar. Look for a thick, fragrance-free cream or ointment containing ceramides, urea, or emollients. These ingredients are proven to help restore your skin’s natural barrier.
To get it right:
- Apply moisturizer to hands, legs, and feet—focus on areas prone to dryness and cracking.
- Skip between the toes to prevent fungal growth.
- Keep a travel-sized tube on your desk or bag for midday touch-ups.
“The right moisturizer is like a protective forcefield for your skin—don’t underestimate its power.”
Cleansing: Gentle, Not Harsh
Harsh soaps and hot showers can strip away precious oils. Instead:
- Use lukewarm (never hot) water and stick to mild, fragrance-free cleansers.
- Shower quickly (under 10 minutes if possible) and avoid scrubbing.
- When drying off, pat—not rub—your skin with a soft towel. Special attention goes to creases and between toes, where moisture can linger and invite bacteria or fungi.
Think of this like tuning a sensitive instrument: small changes in your daily wash routine can keep everything in harmony.
Daily Inspections: Spot Issues Before They Snowball
Checking your skin daily can catch tiny problems before they turn into big ones.
Make it a habit by:
- Using a mirror (or your phone’s selfie camera) to check heels, soles, and under arms.
- Looking for cuts, redness, dry patches, or blisters—especially on your feet.
- Setting a daily calendar reminder or piggybacking the check onto brushing your teeth.
If you spot anything odd—like a blister or a slow-healing sore—don’t wait to ask your healthcare provider for advice. “Daily skin checks are like smoke alarms—a fast warning means faster help.”
Daily moisturizing, gentle cleansing, and quick skin checks aren’t complicated—but for people with diabetes, they’re a proven way to catch issues early and keep your skin strong and healthy, day after day. Adopting these steps is a simple upgrade with long-term payoffs.
Foot Care Fundamentals: Protecting Your Foundations
If you have diabetes, your feet deserve extra attention—think of them as your daily foundation, quietly supporting your every move.
Neglecting them can lead to serious complications, as diabetes affects blood flow and nerve sensitivity—meaning a tiny cut can turn into a trip to the ER if you’re not careful.
Clean and Dry: The Non-Negotiables
Washing your feet every day is a must, but hot water is off the table.
- Use lukewarm water and a mild, fragrance-free cleanser
- Pat dry, don’t rub, especially between toes; moisture there is a magnet for fungal infections
- If you’re picturing missing a spot—try a soft towel or even a hair dryer on a cool setting for those tricky areas
It’s the small details that keep infection at bay.
Make Your Shoes and Socks Work for You
What you put on your feet matters as much as how you wash them.
- Wear supportive, properly fitting shoes to prevent constant rubbing
- Choose clean, soft socks—cotton or moisture-wicking is best
- Avoid tight shoes, sandals, or going barefoot (even at home)—these habits are red flags
- Blisters, calluses, or pressure spots should trigger a pause for inspection
According to recent data, ill-fitting shoes triple the risk of foot ulcers for people with diabetes.
Inspect Like a Pro (No Med Degree Needed)
A daily foot check is your best defense.
- Use your hands for areas you can’t see, or grab a mirror
- Recruit a loved one if needed—two sets of eyes are better than one
- Look for:
- Redness or swelling
- Cuts, blisters, or calluses
- Changes in skin color or temperature
Spotting issues early shuts down serious complications before they start.
Stop Problems Before They Start
Preventing small problems from spiraling saves time, money, and mobility.
- Even a minor injury can lead to major infection due to reduced sensation (neuropathy)
- Report any non-healing wounds or signs of infection to your healthcare team ASAP
- “A quick five-minute check each evening could save you months of recovery—think of it as your daily investment in staying active”
Daily foot care isn’t just about comfort—it’s about preserving your independence and avoiding hospital visits.
Prioritize your foot health and you’ll protect your mobility, boost your confidence, and get one step closer to thriving with diabetes.
Advanced Skin Protection Strategies
Staying ahead of skin troubles with diabetes means thinking beyond just daily routines—it's about anticipating challenges and pivoting with the seasons.
Picture this: It’s January, your office heat is blasting and your skin feels like parchment. Dry winter air draws moisture out faster than you can say “moisturizer”—and your skin barrier needs backup more than ever.
Environmental Factors: Weather-Proofing Your Skin
Combat dry air by:
- Running a humidifier at work or home, especially in colder months. Studies show even a modest humidity boost (up to 40-50%) can ease skin dryness.
- Applying fragrance-free sunscreen (SPF 30+) even on chilly, cloudy days. UV exposure is still a threat in winter and can worsen diabetic skin issues.
- Using nourishing lip balm and protective gloves to safeguard lips and hands from cracking when temps drop or winds pick up.
When summer arrives, sweat and heat can raise your risk for fungal rashes. Think light, breathable fabrics and regular shower breaks after workouts.
Smarter Product Selection: Read, Patch, Prevent
Choosing skincare for diabetes is like selecting software for your workflow—compatibility and security matter.
- Check ingredient lists for minimal, non-irritating formulas (ceramides, urea, emollients; no alcohol or strong scents).
- Patch test new products on a small area—wait 24 hours to watch for redness or itchiness before full use.
- Limit your lineup: The fewer products, the easier it is to spot what works—think quality over quantity.
Handling Minor Irritations: Know When to DIY (and When Not To)
If you spot a small rash, bug bite, or itchy patch:
- Gently clean with mild soap and cool water.
- Cover with a sterile, non-stick bandage.
- Track for change: If it worsens or doesn't heal in a few days, or you notice spreading redness or pus, skip the guesswork and see your doctor.
Over-the-counter hydrocortisone or antifungal creams can sometimes be helpful, but diabetic skin reacts unpredictably—if in doubt, don’t DIY, reach out.
Keeping your skin strong with diabetes means adapting to your environment, choosing smart products, and knowing when a small issue has the potential to become serious. The best move? Treat your skin like an essential interface—keep it secure, updated, and tuned for every season.
The Role of Blood Sugar Management in Skin Health
Keeping blood sugar in check isn’t just about numbers—it’s about keeping your skin strong and resilient. High blood glucose levels draw moisture away from skin cells, leaving you prone to dryness, itchiness, and even slow-healing wounds.
When blood sugar stays elevated, skin loses its natural barrier, making it easier for bacteria and fungi to slip in. Think of your skin like a fortress: if the walls get cracked, invaders can sneak through.
Why Hydration and Diet Matter
You can give your skin daily backup by following three skin-smart habits:
- Drink water consistently: Aim for at least eight cups per day to help cells retain moisture and function normally.
- Eat for stable blood sugar: Choose whole grains, lean proteins, and fiber-rich veggies to avoid spikes and crashes.
- Limit salty and sugary snacks: These can dehydrate you and increase glucose fluctuations, which puts extra stress on your skin.
Picture this: After a long meeting, you reach for water and a crunchy apple, rather than that bag of chips. Your skin (and blood sugar) will thank you for it.
Activity and Circulation: The Skin’s Hidden Helpers
Movement matters, too. Regular exercise boosts circulation, making sure your skin is flush with nutrients and oxygen.
The benefits aren’t just theoretical—studies show people with controlled diabetes reduce skin complication rates by up to 40% compared to those with poor control.
Here’s how to start:
- Walk daily—even short strolls work wonders
- Stretch before bed to promote blood flow overnight
- Take screen breaks to get your body (and skin) moving
Imagine running your hand over your arm and noticing how much softer and more hydrated it feels after a couple of active weeks.
Small Steps, Big Results
Balancing your blood sugar isn’t just good for your next lab report—it’s visible in the health of your skin. Better glucose control means fewer cracks, less dryness, and a stronger natural defense against daily irritants.
Focus on steady routines: drink up, eat smart, move a little each day. These subtle shifts can mean fewer doctor visits and a smoother, more comfortable life with diabetes—starting at skin level.
When to Call in the Pros: Recognizing Serious Skin Concerns
Spotting skin problems early is your best tool for staying ahead of diabetes complications.
Not every itch or scratch needs a doctor—but certain red flag symptoms demand a pro’s attention, fast.
Know Your Red Flags: When DIY Isn’t Enough
Here’s what should send you straight to your healthcare provider:
- Infection warning signs: pus, yellow crust, swelling, or warmth
- Rapidly spreading redness or streaks under the skin
- Fever alongside any skin problem
- Non-healing sores—if a cut or wound won’t close after 7–10 days
- New or worsening foot ulcers, calluses, or blisters
Picture this: You notice a blister on your foot that isn’t shrinking, or redness starts creeping around a small wound. Don’t wait it out—call your provider before things escalate.
Deciding When to Ask for Professional Help
Ask yourself these questions when deciding to manage at home or book an appointment:
- Is the skin issue getting worse despite your usual care?
- Are there signs of infection or severe pain?
- Have you noticed numbness, tingling, or color changes in your feet?
If you answer “yes” to any, that’s your cue.
Social share moment: “If you spot redness spreading fast or a wound that won’t heal, don’t gamble—your skin’s telling you it’s time for backup.”
What To Expect—and How Pros Can Help
When you see a dermatologist, podiatrist, or diabetes educator, you’ll get:
- Expert assessment and advice on safe treatments
- Help with wound care or infection management
- Guidance on custom products or protective gear
- Referrals for advanced therapies if needed
These appointments typically last 20–40 minutes, and the American Diabetes Association recommends annual skin checks—more often if you have recurring issues.
Individualized Care Really Does Matter
No two people manage skin with diabetes the same way.
- Your doctor can tailor advice for stubborn or unusual problems
- Personalized plans mean fewer complications and better outcomes
- The right referral saves time and helps you avoid serious setbacks
Empowering tip: Treat your skin like a report card—share changes and concerns with your care team before they become emergencies.
For anyone with diabetes, keeping a close eye on skin changes and knowing when to call for help is a smart investment in your long-term health and comfort.
Conclusion
Prioritizing your skin health when living with diabetes isn’t just smart—it’s a real advantage you can act on every single day. The right habits become your first line of defense, keeping minor irritations from turning into costly complications and helping you feel your best, both at work and in life.
A few small, consistent choices deliver the biggest impact. With a simple routine and the same attention you give to your devices or deadlines, you can protect your skin, boost your comfort, and stay a step ahead of surprises.
Here’s how to put these tips to work right now:
- Moisturize every day, especially after washing, with a fragrance-free, nourishing cream.
- Inspect your skin and feet daily—a quick glance at trouble spots can prevent trouble later.
- Choose gentle cleansers and skip hot showers to protect your skin’s natural barrier.
- Watch for warning signs like redness, slow-healing cuts, or swelling, and reach out to your care team early.
- Keep blood sugar steady with hydration, movement, and smart nutrition—your skin will show the results.
Ready for immediate momentum? Pick one new habit from above, set a reminder on your phone, and make it part of your daily workflow. Share the best tip with a friend who can use it—your smarter skin care routine might be the inspiration they need too.
Your skin is your daily interface with the world—invest in simple, proactive care, and you’ll turn prevention into real power. Healthy skin isn’t just possible with diabetes. It’s absolutely within your reach.
“Pay attention to your skin today, and you’ll set yourself up for a stronger, more comfortable tomorrow—one confident step at a time.”