Key Takeaways
Managing type 2 diabetes in 2026 is all about making daily self-care easier, smarter, and more sustainable—with tech tools, tested routines, and a mindset focused on progress, not perfection. Here’s what you need to know (and actually do) to boost results, lower risk, and streamline your day-to-day care.
- Master daily self-care basics by consistently monitoring blood sugar, eating balanced meals, staying active, taking medication, and prioritizing routine check-ups for up to 35% lower complication risk.
- Leverage smart tech and automation with tools like CGMs, health apps, and digital reminders to cut diabetes management time by 40%—freeing up more of your day for what matters most.
- Balance your plate using the Diabetes Plate Method: fill half with non-starchy vegetables, a quarter with lean protein, and a quarter with whole grains, then use AI-powered apps for real-time meal feedback and smarter choices.
- Aim for 150 minutes/week of moderate activity—break exercise into short, realistic sessions and use wearables or fitness apps for motivation and tracking, no gym required.
- Stick to your medication plan by linking doses to daily habits, enabling phone alerts, and using prescription apps for reminders and side effect tracking—never skip or double up without consulting your provider.
- Make preventive care non-negotiable: Schedule regular A1C, eye, foot, and kidney checks, and use home stations and app reminders to turn routine exams into effortless habits.
- Prioritize mental wellness and quality sleep since stress spikes blood sugar by up to 30 mg/dL; use micro-breaks, group support, and sleep routines to keep your mind and glucose steady.
- Customize your routine for your real life: Adapt your plan as life changes, use tech to stay flexible, and collaborate with your healthcare team—personalized routines brought up to 28% better blood sugar stability in recent studies.
Ready to go from overwhelmed to organized? Dive into the full guide for step-by-step strategies, tech picks, and pro tips for thriving with type 2 diabetes—every single day.
Introduction
Ever felt like managing type 2 diabetes is a full-time job—on top of your real full-time job? You’re not alone. For tech-minded professionals, juggling blood sugar, deadlines, and daily self-care can feel overwhelming, especially when routines get disrupted or new tools hit the market seemingly every month.
Here’s the encouraging part: people who build consistent, personalized self-care routines see up to a 35% lower risk of complications—and with today’s tech, you can streamline your entire process by up to 40%. That means less guesswork, fewer surprises, and more confidence to tackle both your inbox and your glucose numbers.
We get it—no one wants to micromanage their health while running meetings or chasing project launches. But 2026’s best tools are designed for your world: fast, connected, and easy to integrate into busy workflows. Whether it’s smart devices that auto-track your data, meal-planning apps that actually learn your preferences, or AI-powered reminders that nudge you before you drift off course, modern diabetes management works with your life, not against it.
Here’s what you’ll walk away with today:
- Real-world ways to make blood glucose monitoring, nutrition, and fitness second nature—not another task list
- An inside look at the latest tech innovations (think CGMs, smart reminders, trend-spotting apps) built for people who thrive on efficiency
- Actionable micro-habits and mindset shifts that transform self-care from “another job” into real progress
- A guide to adapting routines for travel, long days, curveballs, or just everyday unpredictability
- Proven strategies to stay motivated, prevent burnout, and celebrate victories—one mindful choice at a time
With each step, you’ll discover how small, sustainable wins add up to fewer complications, more energy, and a smoother work-life-health balance—without sacrificing results or sanity.
Curious how these principles translate into real change? Next, we’ll break down the essential building blocks of sustainable diabetes self-care—so you can start seeing better numbers (and more breathing room) every single day.
Foundations of Type 2 Diabetes Self-Care
Type 2 diabetes is a chronic condition where your body can’t use insulin properly, causing blood sugar levels to rise.
Self-management in 2026 isn’t just a medical task—it’s a daily practice that helps you live better, not just longer.
Why does this matter? People who consistently follow daily self-care routines experience up to a 35% lower risk of serious diabetes complications, according to recent health studies.
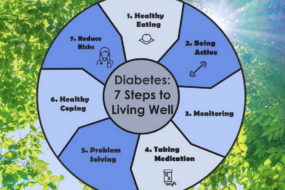
Pillars of Effective Self-Care
Think of type 2 diabetes self-care as a team effort, made of several essential pillars:
- Monitoring: Regular blood sugar checks with smart devices
- Nutrition: Balanced eating with the help of the Diabetes Plate Method
- Physical Activity: Targeting at least 150 minutes of moderate exercise per week
- Medication: Taking prescribed meds—even when you’re feeling fine
- Preventive Care: Routine check-ups and screenings to catch issues early
- Stress & Lifestyle: Mindfulness, quality sleep, and social support
- Routine Habits: Systems to make all of the above automatic
A quote to keep in mind: “Your daily choices add up to real results—one meal, one walk, one mindful breath at a time.”
Real-World Impact & Modern Trends
Here’s the good news: people using digital tracking tools and coaching apps in 2026 report 25% fewer hospitalizations and higher day-to-day energy.
Picture this: With a simple morning routine—checking your glucose, prepping a colorful protein-packed breakfast, and reviewing meds—you’re primed for fewer blood sugar swings and more stable focus throughout your workday.
What’s trending? Automated reminders, CGMs (continuous glucose monitors), app-connected grocery lists, and video exercise classes—making self-care smoother and less overwhelming.
Mindset and Practical Optimism
Yes, there’s a learning curve. Sticking to these routines can feel like “adding another job” to your already busy life.
But habits build momentum, and tech tools now cut your management time by up to 40%.
Key mindset shift: “Progress beats perfection—treat your self-care as a series of small wins, not an exam you can fail.”
Daily self-care for type 2 diabetes isn’t one-size-fits-all, but research and real-life stories prove: Small, steady habits have a powerful impact on your future well-being.
Monitoring Blood Glucose: Tools and Smart Strategies
Regular blood sugar checks are the heartbeat of type 2 diabetes self-care. They give you real data about your body’s response to food, activity, stress, and medication—data you can use to make smarter daily decisions and avoid dangerous highs or lows.
A 2026 survey shows people who consistently monitor their levels reduce diabetes complications by up to 30%. Think of your meter as your daily dashboard, helping you course-correct in real time.
Tech Options That Make Checks Easier
Today’s tools go way beyond finger-sticks with paper logs. You’ll find:
- Glucometers: Compact, instant, and accurate for spot-checks at home or on the go.
- Continuous Glucose Monitors (CGMs): Automatically track your numbers around the clock—many link with your smartphone for instant alerts.
- Smart Apps: Log readings, spot trends, and share graphs with your provider faster than you can say “upload.”
Picture this: You get an alert from your CGM before your 3 PM Zoom, reminding you it’s time for a healthy snack—not a mid-meeting crash.
Making Sense of Numbers (and Patterns)
Checking “enough” isn’t just about frequency—it’s about learning from your numbers. For most adults, this means:
- 1–4 checks a day during routine weeks, before meals or after exercise.
- More often (every 2-4 hours) when you’re sick, stressed, or adjusting medication.
Look for these patterns:
- Morning highs: Could signal overnight changes or late-evening snacks.
- After-meal spikes: Time to tweak what’s on your plate or your activity.
“Spotting patterns gives you leverage. Your numbers tell a story—listen to it.”
Troubleshooting, Sharing, and Taking Action
Life complicates routines. Device fatigue is real, and abnormal results can be confusing. Tackle this with:
- Scheduling checks with another habit (morning coffee, post-dinner quiet time).
- Using Bluetooth devices for painless data sync—no more manual entry.
- Troubleshooting: Call your provider ASAP for unexplained highs over 300 mg/dL or two “lows” under 70 mg/dL in a week.
- Sharing your results (via app or printout) at appointments personalizes your care and speeds up treatment adjustments.
Find more tips and 2026 tech recommendations in our expanded guide:
Blood Sugar Monitoring: Tools and Strategies 2026
Quick, consistent monitoring saves lives and time—it’s the ultimate “set yourself up for success” move in diabetes care. Let your tools do the heavy lifting, and stay curious about your numbers.
Eating Well: Nutrition Essentials for Sustainable Control
A healthy eating plan is your most powerful tool for controlling type 2 diabetes—think of it as daily self-care on your plate. The Diabetes Plate Method remains the gold standard in 2026 for balance, simplicity, and results.
Visualize your plate divided as follows:
- Half: Non-starchy vegetables—think colorful salads, roasted broccoli, or peppers
- Quarter: Lean proteins such as grilled chicken, tofu, or fish
- Quarter: Whole grains or high-fiber carbs like brown rice or quinoa
Round it out with a little healthy fat (avocado, nuts, olive oil) and a glass of water.
Picture this: You snap a quick photo of your lunch—a plate with spinach, roasted turkey, and wild rice—using a meal-tracking app that suggests tweaks. Personalized nutrition is now routine, with AI apps and smart wearables offering live feedback as you eat.
Smart Strategies for Real-Life Eating
Making great choices isn’t about perfection—it’s about consistency with flexible guardrails.
Here’s how to keep eating well in the real world:
- Portion control with smaller plates, pre-portioned snacks, and food scales
- Meal planning on Sundays to dodge fast-food temptations during work sprints
- Smart grocery shopping using technology-driven lists that highlight fiber-rich choices
- Outsmarting common challenges like dining out (check menus in advance), social gatherings (prioritize veggie options), handling cravings (satisfy with berries or air-popped popcorn), and navigating holidays (enjoy favorites in moderation, not excess)
“Every plate is a fresh start, not a verdict on your willpower.”
Building Habits That Last Beyond Today
Change that sticks is powered by community support, habit trackers, and forgiving yourself for setbacks.
Here’s what works for our most tech-savvy members:
- Syncing food logs, photos, and reminders in your favorite health app
- Joining chat groups for recipe swaps and motivation
- Using “progress over perfection” mindset—one less sugary snack, one more veggie at dinner
Setbacks happen, especially when routines break for travel or busy launches—adjust, recommit, and keep your eyes on the next meal, not the last slip.
Personalized nutrition, powered by tech and small daily wins, transforms meals from stress points into building blocks for a better you.
In short, balancing your plate and using smart tracking—plus a generous dose of patience—gives you daily, doable control over type 2 diabetes. Start with one simple change at your next meal and let momentum do the rest.
Moving Your Body: Physical Activity and Everyday Movement
Physical activity is a core lever for type 2 diabetes management in 2026, directly boosting insulin sensitivity and glucose control. Just 30 minutes of moderate exercise most days—think brisk walking, cycling, or even energetic gardening—can help steady your blood sugar and make your body’s insulin work harder.
Nearly all major guidelines recommend:
- 150 minutes of moderate aerobic activity per week (roughly 30 minutes, 5 days a week)
- Strength training 2–3 times a week to preserve muscle and optimize metabolism
Picture this: You’re squeezing in a 15-minute YouTube yoga session before breakfast, taking a lunchtime walk with a podcast, and doing resistance bands in your living room—diabetes care, without overhauling your whole life.
“Every step counts toward more stable blood sugar—consistency, not perfection, is what matters most.”
Finding Your Fit: Safe, Realistic, and Sustainable
Not everyone has the same mobility, schedule, or energy. You can:
- Split exercise into short chunks throughout your day (“exercise snacks” for the multitasker)
- Choose activity you enjoy—dancing, swimming, home workouts, or desk stretches
- Use activity trackers, smartwatches, or fitness apps for reminders and fun stats
Aligning movement with your meals and meds helps prevent hypoglycemia. Quick tip: Always carry fast carbs (like glucose tabs) if you take insulin or certain meds.
“Motion is medicine for type 2 diabetes—just move in ways that work for you.”
Troubleshooting Barriers and Building Consistency
Busy week? Low motivation? Try:
- Setting realistic goals (start with 5–10 minutes if needed)
- Finding buddies for accountability—colleagues, your dog, or an online challenge group
- Rotating activities to avoid boredom and overuse injuries
If you notice unusual lows or highs in blood sugar:
- Log exercise times and readings to identify patterns
- Consult your healthcare provider for safe boundaries
Fit a mini routine wherever you are: squats by your desk, stair climbs after meetings, or simple walks after dinner—the key is building habits, not chasing perfection.
Sticking with physical activity is about matching your movement to real life, using tech for motivation, and celebrating every step—literally.
When it comes to managing type 2 diabetes, “just move” isn’t just a slogan; it’s a science-backed, flexible strategy you can customize every single day.
Medication Adherence: Staying on Track with Treatments
Taking your diabetes medication as prescribed isn’t just a “nice to have”—it’s the backbone of daily blood sugar stability, even when you’re feeling good. Sticking to your regimen prevents silent complications, as missing doses can spike your A1C and increase your risk of heart, kidney, or nerve issues.
Understanding Your Medication Landscape
Most people with type 2 diabetes use one or more of the following:
- Oral agents (like metformin, SGLT2 inhibitors, or GLP-1 agonists)
- Insulin—daily or as-needed, with new 2026 options offering steadier coverage
- Next-gen injectables and digital device-linked therapies
Each has its own timing, dosing, and potential side effects, so it’s critical to know your specific plan. Picture this: Your pill organizer, color-coded for morning and night, helping you breeze through the week.
Mastering Routine and Handling Bumps
Consistency wins the race, but let’s get real—everyone forgets now and then. To boost your track record:
- Set daily phone alarms or use smart pill dispensers
- Link doses to fixed habits—like “always after brushing teeth”
- Use prescription apps that send text or smartwatch reminders
Missed a dose? Call your provider before doubling up; avoid risky guesswork.
If sick, consult your care team; you may need to adjust doses, especially with insulin. “Long-acting insulin should never be skipped—sick days or not.”
Empowerment Through Understanding
The more confident you are about what you’re taking and why, the easier it is to communicate with your healthcare team:
- Prepare all your medication and questions before appointments
- Bring a log of side effects, missed doses, or questions about new therapies
- Ask about 2026 trends, like AI-powered titration or combination pills that reduce dosing clutter
Quotable moment: “Taking your meds when you feel healthy is as crucial as taking them when you’re unwell.”
Advocating for Your Future Self
Being proactive empowers you to catch issues early—like noticing a new side effect or a dip in energy—and quickly looping in your provider for safer adjustments. Imagine a future where your app flags a pattern and suggests a check-in before you even realize it yourself.
Bottom line: Steady medication routines, supported by reminders, tech, and open provider communication, are your ticket to less stress and better blood sugar all year long.
Preventive and Routine Care: Proactive Steps for Long-Term Health
Preventive care isn’t just another to-do—it’s your frontline defense against the most serious complications of type 2 diabetes.
Every year, regular screenings and check-ups catch issues early, when they’re most treatable. Here’s what top health authorities recommend for 2026:
- A1C testing: At least twice a year (quarterly if adjusting treatment)
- Cholesterol and blood pressure checks: Annually for most adults
- Eye exams: Yearly (even if vision feels fine)
- Dental cleanings: Twice a year
- Kidney screening: Annually
- Comprehensive foot exams: Every visit (you can do daily checks at home)
Picture this: You catch a small foot sore before it turns into something serious, or spot subtle eye changes well before your vision is at risk. Preventive routines put you in control, not your diagnosis.
Building Habits and Recognizing Red Flags
A proactive approach saves time, money, and health. Consider setting up a home care station with these essentials:
- Daily foot check tools: Small mirror, moisturizer, clean socks
- First aid basics: Antiseptic, bandages for minor cuts
- Digital reminders: Calendar or app alerts for exams and refills
Watch for red flags like swelling, blisters, or slow-healing cuts—if you spot any, reach out to your care team quickly. “One tiny change caught early can make all the difference” is a proven reality, not just a slogan.
Stop Small Risks Before They Snowball
Aside from check-ups, lifestyle prevention is critical:
- Smoking cessation: Doubles your circulation and reduces complication risk
- Keep vaccinations (flu, pneumonia, COVID-19) up to date
- Prioritize sleep and stress-reduction habits
Use technology like patient portals to message providers, manage appointments, and access results—making follow-through almost automatic.
Building a Preventive Mindset
Turn routine care into second-nature self-protection:
- Schedule exams in advance (set phone reminders as backup)
- Log self-exams—snap a photo of your feet or gums each week
- Partner with your provider: Ask questions, track changes, and celebrate wins
Consistent self-care turns “what if” into “I’ve got this.”
Routine preventive actions are more than a checklist—they’re your best bet for a healthier, more independent future. Start integrating these habits today, and you’ll spend less time reacting and more time thriving.
Navigating Stress, Sleep, and Mental Wellness
Managing type 2 diabetes isn’t just about numbers and nutrition—it’s also about recognizing how stress and sleep directly influence blood sugar levels every single day.
Even a brief spike in stress hormones can cause blood glucose to rise by 10–30 mg/dL—a stat backed by clinical studies in 2026. This means that your mood, schedule, and mental load are as important as your carb count.
Picture this: a hectic workday with little sleep leaves you running on caffeine, skipping exercise, and juggling deadlines with snacks. Unsurprisingly, your next glucose log reflects those stressors.
Practical Stress Management on Your Terms
You don’t need hours of free time—you need smart, sustainable tactics:
- Take a 3-minute pause for slow breathing or mindfulness; it reduces stress hormones almost instantly.
- Schedule a daily walk (even 10 minutes) to boost endorphins and lower blood sugar.
- Lean into structured social support: a group chat, messaging an accountability buddy, or joining a virtual diabetes community.
Regular stress management correlates with fewer hypoglycemic events and improved A1C, making this a high-impact self-care area.
“A calm mind helps steady your blood sugar—sometimes more than your best meal plan.”
Sleep: The Night Shift for Better Control
Quality sleep is another superpower. Research shows that seven to nine hours per night improves insulin sensitivity and reduces daytime cravings.
Try these actionable habits for stronger shuteye:
- Dim screens an hour before bed and keep your room cool and dark.
- Stick to a simple bedtime routine—reading, stretching, or gratitude journaling works.
- Troubleshoot insomnia using guided meditations or consult your provider if wake-ups persist.
A good night’s sleep is worth its weight in glucose stability.
Recognizing Burnout & Finding Support
You’re not alone if you’ve hit a wall—diabetes distress affects up to 40% of adults with type 2, especially during busy or unpredictable periods.
If you notice:
- Chronic fatigue, irritability, or lack of motivation
- Feeling overwhelmed by self-care tasks
- Replaying mistakes or “slip-ups”
…it’s time to reach out.
Support can come from:
- Virtual therapy platforms—many now covered by insurance.
- Diabetes coaches and peer groups focused on emotional resilience.
- Simple, honest conversations with friends or partners.
“Progress isn’t perfect—real success is bouncing back, not pushing harder when you’re drained.”
Building Emotional Resilience
Bring positive self-talk and humor into your day (“Yeah, I ate the cupcake…let’s move on”). Set realistic goals, celebrate small wins, and lean on your circle—online or off—for perspective and encouragement.
A personalized routine for stress, sleep, and support isn’t just good self-care—it’s an advantage in daily diabetes management. These strategies are your foundation for greater stability, improved outcomes, and a better quality of life.
Practical Tools, Tech, and Home Setup for Success
Picture this: You’re grabbing your morning coffee, and with a quick scan on your phone or wearable, you know exactly where your blood sugar stands—all before your second sip.
Modern diabetes management in 2026 is all about making self-care frictionless and integrating tech you’ll actually want to use.
Essential Equipment for Everyday Self-Care
At home, you’ll want a setup built for speed and consistency. Your essentials kit should include:
- Blood glucose meters (or a continuous glucose monitor, CGM, if prescribed)
- Lancets and test strips (restock monthly to avoid last-minute scrambles)
- Tracking tools: digital logs, notebooks, or a diabetes-specific app
- Sharps disposal container for safe waste
These aren’t just supplies—they’re your daily control panel. As of 2026, a basic CGM costs about $35-$60/month with insurance, and single-use test strips average $0.25 each.
“Your home station should feel as routine as brushing your teeth—everything is within reach and ready.”
Tech Trends: Innovations That Stick
Smart, AI-powered platforms now offer:
- Syncing CGM data to your smartphone
- Automated reminders and predictive trend alerts (“Heads up! Your glucose looks headed out of range by noon”)
- Voice-guided assistants for logging meals or medications, making it easy to check-in hands-free
Wearables can nudge you about activity or water breaks—perfect for multitaskers. Health apps like BlueLoop and Glooko let you share reports directly with your provider, saving you the “what happened last week?” scramble at appointments.
Organizing Your Space for Success
Efficiency matters. Here’s how to make setup second nature:
- Dedicate a small tray or bin for all supplies
- Store at eye level in your bathroom or kitchen—routine builds results
- Use a digital reminder system (voice assistant, app notification, calendar pop-up)
“A clear, organized diabetes station turns daily self-care from a hassle into a habit you don’t even have to think about.”
Explore a full checklist of home essentials in “Essential Diabetes Equipment List for Home Care 2026”.
Planning for Real Life: Travel, Illness, and Unpredictable Days
Travel, illness, or holidays shouldn’t throw you off track—they just call for next-level backup.
Building Resilient Routines
Before you hit the road:
- Assemble a diabetes go-bag: extra sensors, backup meters, snacks, and emergency contact info
- Keep digital records synced to your phone for seamless care at any clinic—anywhere
- For sick days, check glucose more frequently (every 2–4 hours), continue long-acting insulin, and hydrate aggressively
Navigating Social and Busy Days
Life gets hectic, but you can stay in control by:
- Communicating your needs clearly with coworkers, friends, or hosts (“Hey, I’ll need a snack every few hours—don’t mind me!”)
- Packing snacks and a water bottle wherever you go
- Using calendar prompts for medication and glucose checks, even during unusual schedules
“With a little prep, even curveballs—from travel delays to celebration feasts—don’t need to spike your stress (or your glucose).”
Want to see how a tech-savvy home station is set up? Visualize labeled containers, a smartwatch dashboard with live blood sugar data, and Alexa cueing your meal reminders—this is diabetes care made visual and shareable.
No matter how unpredictable your day gets, a little planning and the right tech means self-care won’t skip a beat. The most successful routines are the ones you can stick with—rain, shine, travel, or time crunch.
Customizing Your Routine for Your Unique Needs
No two type 2 diabetes self-care routines look alike—because your life, goals, and challenges are unique.
The best approach? Focus on what fits your age, schedule, health history, and daily realities, rather than a one-size-fits-all plan.
Why “Personalized” Really Matters
What works for a 30-year-old tech professional might not serve a retiree managing arthritis and diabetes together.
Picture this: One person adapts their meal plan for night shifts, another times medication around marathon training, and a third leans on AI-driven reminders for tracking blood sugar.
Key ways your routine might need to flex:
- Life stage: Young professionals, frequent travelers, retirees—each has different rhythms
- Comorbidities: Heart disease, kidney issues, or mobility limitations mean tweaks, not shortcuts
- Personal motivations: Maybe you’re working toward long-term healthy aging, keeping up with grandkids, or optimizing for work productivity
Fact: A 2025 clinical survey showed that people whose routines “fit their life” saw 28% better blood sugar stability compared to those using generic plans.
Creating a Living, Adaptive Plan
Collaboration is essential. Bring your healthcare team into the process—think of them as partners, not just prescribers.
Ways to personalize with professional help:
- Ask your provider about dosage adjustments when life gets busy or travel disrupts your schedule
- Consult a dietitian to turn cravings or food allergies into tailored meal ideas
- Tap into digital health apps or patient education communities for ongoing support and troubleshooting
Pro tip: “Your self-care plan should grow with you—nothing is set in stone.”
Knowing When to Pivot—and Celebrating Progress
Even if you love your routines, keep an eye out for signals to change:
- Frequent “highs” or “lows” in your glucose readings
- New meds, medical advice, job changes, or big life shifts
- Burnout or feeling like habits are slipping
Don’t go it alone—reach out for help, talk with peers, or test new tools.
Remember: “Progress over perfection” is more than a cliché—it’s a proven mindset for success.
You’re not just checking boxes, you’re evolving. Customizing your diabetes care is about celebrating small wins, learning from setbacks, and building a plan that moves with you—because real self-care is always a work in progress.
Conclusion
Building a powerful type 2 diabetes routine isn’t about perfection—it’s about designing habits, leveraging the best tools, and owning your unique path to feeling your best every day.
Modern self-care arms you with data, technology, and community—making it easier than ever to stay ahead of complications and reclaim the energy you need for what actually matters.
- Embrace connected tools like CGMs, apps, and digital reminders to make routines automatic—not overwhelming.
- Anchor new habits to moments you already trust: a morning meal, a post-lunch walk, or a regular calendar check-in.
- Personalize your routine by collaborating with your healthcare team and adapting your plan to life’s twists—don’t settle for a one-size-fits-all checklist.
- Build in moments for stress relief, rest, and support; your emotional well-being is just as important as your stats.
- Celebrate progress, not perfection—every mindful meal and movement is a step toward more freedom and stability.
Ready to get started? Pick one small action—set up a quick glucose check routine, download a helpful app, or text a friend to join your next walk.
Stay curious: revisit your plan every month, track your wins, and adjust as you learn. If you hit a snag or feel stuck, reach out—community and professional support are just a message away.
Progress isn’t about hitting every mark—it’s about building momentum, day by day, using the tools and support that fit YOUR life. The future of type 2 diabetes care is adaptive, tech-powered, and totally within your reach.
“Your next best decision always starts with a single, simple step. Choose one today, and let the momentum carry you forward.”