Key Takeaways
Menopausal joint pain isn’t just about getting older—it’s a direct response to hormone shifts, with over half of midlife women feeling the impact. Understanding the root causes and science-backed solutions empowers you to take smart, actionable steps for relief. Here’s what you need to know, fast:
- Estrogen drop is the root trigger for joint pain in menopause, driving up inflammation, stiffness, and aches—especially in your knees, hips, hands, and spine.
- Over 50–70% of women experience new or worsening joint pain during perimenopause and postmenopause, making this a mainstream, not marginal, symptom.
- Estrogen normally acts as a built-in joint protector: it keeps cartilage strong, lubricates joints, and calms inflammation—its decline amplifies pain signals and joint wear.
- Hormonal shifts cause “invisible” pain that doesn’t always show on X-rays but feels very real, with symptoms like morning stiffness, diffuse aches, and unpredictable flares.
- Aging, weight gain, and inactivity amplify joint pain; every extra pound adds up to 4x more pressure on your knees, so maintaining movement is key.
- Lifestyle tweaks deliver real relief: regular gentle exercise, strength training, anti-inflammatory foods, and weight management can break the pain–inactivity–pain cycle.
- Hormone therapy and targeted non-hormonal options (like NSAIDs, supplements, or physical therapy) may reduce pain—personalize your approach based on your root causes.
- If joint pain is sudden, severe, or comes with red flags (like redness, swelling, fever, or single-joint pain), get checked to rule out other conditions—don’t just chalk it up to menopause.
Knowing why joint pain flares during menopause is your first step toward choosing smarter, root-cause solutions. Dive into the full article for practical strategies and personalized action plans to get moving comfortably again.
Introduction
Wake up feeling like your joints have aged a decade overnight? You’re not just imagining things. Over 70% of women in midlife report their knees, hips, or hands suddenly creak, ache, or stiffen as menopause sets in.
If you’ve noticed joint pain ramping up just as hot flashes or sleep glitches begin, you’re in good company—this frustrating shift is a real, common, and misunderstood piece of the menopause puzzle.
Why does it happen now, and not just as a slow drift with age? The answer lies in the sudden hormonal shake-up that comes with menopause—especially the drop in estrogen. These changes don’t just affect mood or metabolism; they spark a chain reaction in your joints, making the discomfort impossible to ignore.
Here’s what you’ll walk away with:
- Clarity on why menopause uniquely triggers joint pain (spoiler: it’s not just “getting older”)
- Actionable strategies to address the real root—not just mask the symptoms
- A checklist of red flags to know when joint pain needs extra attention
- Insights that tie science to practical, everyday solutions—so you can advocate for care that fits your needs
This isn’t about powering through or chalking it up to bad luck. It’s about understanding the biology behind each twinge and finding options that put you back in control.
Ready to see exactly how menopause rewires your joint health—and which levers you can pull to get ahead of the pain? The connection between hormonal changes and joint discomfort is both fascinating and deeply practical.
Let’s break down the science and real-world experiences that finally explain why your joints feel different, starting with the link between menopause and pain that too many women have been told to ignore.
Understanding the Link Between Menopause and Joint Pain
Joint pain isn't just a footnote of getting older—it's a core symptom that shows up loud and clear for many women around menopause.
Picture this: over 50–70% of women in midlife report new or worsening joint discomfort as they move through perimenopause to postmenopause. If your knees suddenly feel creakier, or you wake up each morning with stiff fingers and aching hips, you’re definitely not alone.
Why Does This Happen Now?
It’s not random, and it’s not just age working against you. The surge in joint pain during menopause is absolutely linked to hormonal changes, especially the drop in estrogen.
You'll hear women describe:
- “Morning stiffness that wears off, but only after a hot shower”
- “Joints that feel like they need oiling, especially after sitting”
- “Aches moving from hands one week to knees the next”
These real-world complaints match what clinicians and researchers see in the data. The timing of these symptoms aligns closely with falling estrogen and progesterone levels—not simply years lived.
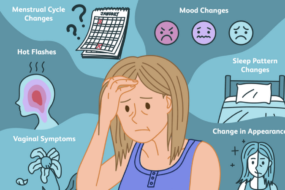
What Makes Menopause Joint Pain Unique?
Unlike standard wear-and-tear arthritis, menopausal joint pain often hits suddenly, feels more generalized, and is paired with other symptoms like night sweats or sleep trouble. The joints most commonly affected include:
- Knees and hips (weight-bearing)
- Hands and wrists (fine motor)
- Spine and lower back
In many cases, imaging scans are normal, which means the pain feels real but isn’t always matched with dramatic changes on X-rays. This “invisible” nature can make it extra frustrating.
Major Trends and Actionable Takeaways
Here are three things worth remembering:
- Over half of women in midlife will experience joint pain around menopause—you’re genuinely in the majority.
- If your joint discomfort started with hot flashes or irregular periods, hormonal changes are likely playing a starring role.
- Recognizing menopausal joint pain can help you target the root cause, not just treat the symptoms.
When joint pain arrives during menopause, it’s not “all in your head”—it’s a powerful, widespread biological shift. Knowing this is the first step toward relief and smarter care decisions.
The Role of Estrogen: How Hormones Protect Joint Health
Estrogen Basics and Its Influence on the Body
Think of estrogen as the oil in your body’s engine—it keeps everything gliding and reduces friction between moving parts.
This hormone delivers its magic by:
- Maintaining bone strength and density
- Supporting healthy, flexible cartilage in your joints
- Boosting production of synovial fluid (that’s the natural lubricant for your joints)
Estrogen’s anti-inflammatory powers are legendary. It calms swelling and helps regulate your body’s pain response. When this hormone is balanced, joints move smoothly and aches stay in check.
“Estrogen is the body’s built-in joint protector.”
“If you’ve ever wondered why teenage athletes bounce back from falls, thank their estrogen levels.”
Estrogen Decline During Menopause
Around perimenopause and postmenopause, estrogen levels drop sharply—sometimes in unpredictable waves, sometimes in a sudden free fall.
- This hormonal rollercoaster typically hits women in their late 40s to early 50s
- Progesterone, another key hormone, also grinds lower and loses its pain-dampening effects
It’s not just estrogen alone; the hormonal duo works together to soften pain and keep tissues resilient.
Imagine a well-oiled machine suddenly running dry—parts squeak, grind, and slow down.
What Happens to Joints When Estrogen Drops
When estrogen declines, the following chain reaction unfolds:
- Inflammation ramps up—higher levels of cytokines like TNF‑α create more swelling, stiffness, and that classic “morning rust”
- Cartilage breaks down faster, raising your risk of osteoarthritis by up to 40% in some joints
- Joint lubrication dries out so you may notice more creaks, cracks, and uncomfortable friction
- Your pain sensitivity rises—even ordinary aches feel more intense due to shifts in how your brain processes pain
Picture this: You wake up and your knees click, your fingers feel stiff, and your muscles ache more than they used to—all because estrogen isn’t there to cushion the impact.
Here’s the takeaway: Estrogen’s steady presence is key to joint comfort. Its decline during menopause triggers a domino effect—fueling inflammation, drying out joints, and leaving nerves more reactive to pain. Understanding this change gives you the power to target relief right at the root.
The Biological Chain Reaction: From Hormones to Joint Pain
Inflammation Escalates
When estrogen begins its dramatic decline during menopause, your body’s natural pro-inflammatory pathways swing into high gear.
Think of it like flipping a switch—higher levels of inflammatory markers such as TNF-α show up in the blood, leading to:
- Swelling and joint stiffness, especially in the morning
- That classic “rusty” or achy feeling when you first get out of bed
Nearly 70% of women in perimenopause report these “stiff-start” mornings—picture yourself pausing before your first cup of coffee, joints not quite ready for action.
“Menopausal joint pain is not just age; it’s an inflammatory shift happening under the hood.”
Cartilage, Bone, and Joint Structure Changes
Estrogen is a key “maintenance manager” for cartilage and bone.
As levels drop, you get:
- Faster cartilage wear-and-tear—hello, more creaking and less shock absorption
- A spike in osteoarthritis rates: Postmenopausal women see osteoarthritis risk climb by up to 25%
- Bone density loss (osteopenia, then osteoporosis), which shifts how weight and impact are absorbed by joints
Suddenly, everyday movements stress your joints and supporting tissues more than before.
Synovial Fluid and Joint Lubrication
Estrogen keeps the synovial fluid—your natural “joint oil”—flowing smoothly.
When estrogen wanes, expect:
- “Drier,” more creaky or sticky joints
- More frequent popping or crunching noises
- Discomfort that feels like your hinges need WD-40
Mild popping is normal, but persistent swelling or heat warrants attention.
Muscle, Ligament, and Tendon Impact
Muscles and soft tissues need estrogen too.
With loss comes:
- Accelerated muscle loss (sarcopenia)
- Weaker support for already stressed joints
- Reduced flexibility and a higher chance of tendon and ligament injuries
Think of trying to support a bridge with fewer and weaker cables—a recipe for tension and trouble.
Central Pain Processing and Sensitivity
Finally, declining estrogen and progesterone rewire your pain experience.
Pain signals get amplified, so:
- The same joint change feels much sharper and more intense
- Mood and sleep challenges can further jack up your pain sensitivity
“Menopausal pain can feel outsized—not because you’re imagining it, but because your nervous system is fired up.”
Understanding this chain reaction gives you power: joint pain during menopause isn’t random, and knowing the triggers helps you target the right relief—whether that means lifestyle tweaks, medical care, or both.
Beyond Hormones: The Role of Aging, Weight, and Lifestyle
The Cumulative Effect of Aging
Menopause doesn’t happen in a vacuum—midlife joint pain is often a tag-team effort between hormonal dips and good old-fashioned aging.
By your late 40s and 50s, joint “wear and tear” is already gaining speed. That familiar morning stiffness or snap-crackle-pop in your knees? It’s your cartilage thinning and bones feeling the grind, a process called osteoarthritis that ramps up with age.
For many, menopause marks the intersection of:
- Natural cartilage breakdown
- Declining muscle mass
- Past injuries resurfacing
Imagine: One morning, you notice your hands feel stiff opening a jar—aging and hormones just joined forces.
Weight Gain and Metabolic Shifts
Here’s a statistic to chew on: Most women will gain 5–10 pounds around menopause, and the weight likes to settle where it puts the most stress on your joints.
Why does this matter? Every extra pound adds roughly 4 pounds of pressure to your knees, making daily movement harder and discomfort more likely.
There’s a vicious cycle to watch for:
- Estrogen drops, triggering weight gain (often around your belly and hips)
- More weight = more joint strain, especially in your knees, hips, and spine
- Pain makes you less active, causing stiffness and further weight gain
Think of it as a domino chain—one factor tips, and the rest tumble fast.
Physical Activity and the Vicious Cycle
When joint pain kicks in, it’s tempting to slow down—but inactivity is joint pain’s best friend.
Reduced movement:
- Accelerates muscle loss (sarcopenia)
- Stiffens joints, amplifying pain with every step
- Makes even gentle exercise feel more daunting over time
Picture this: Skipping walks for a week can quickly lead to major stiffness. Yet, motion is the only way to “oil” those creaky joints.
The big takeaway? Hormones matter, but lifestyle and age-related changes turn up the volume on menopausal joint pain. Staying active, even in small ways, keeps the cycle from spiraling out of control. If you can move—even a little—you'll preserve strength, mobility, and comfort for years to come.
Evidence for Estrogen’s Direct Impact on Joint Pain
What the Research Shows
Nearly 70% of women in midlife report new or worsening joint pain right around menopause.
This isn’t just background noise—research consistently shows a clear spike in joint symptoms during the menopausal transition, with aches, stiffness, and morning discomfort hitting hardest in early postmenopause.
Studies reveal striking patterns:
- Most women notice joint pain peaking in the years right after periods stop
- Sudden changes—like halting hormone therapy (HRT) or starting aromatase inhibitors for breast cancer—cause joint pain flare-ups within weeks
- Joint complaints are often reported even when medical imaging looks “normal,” suggesting a biochemical—not purely structural—origin
Think of your joints as sensitive weather vanes: when estrogen drops, symptoms rise.
What Treatment Trials Reveal
The question isn’t just “do women hurt more after menopause?” It’s, “does estrogen actually protect joints?”
Large trials offer useful clues:
- The Women’s Health Initiative—a study tracking tens of thousands of women—found that those who received estrogen alone post-hysterectomy saw a modest but lasting decrease in joint pain
- Similar research with hormone therapy shows that joint pain frequency drops in women using estrogen, especially if started around menopause
Translation: Estrogen therapy doesn’t cure joint pain, but for certain women, it does take the edge off—and those effects build a strong case for a cause-and-effect link.
These findings are actionable: “If you’re seeing sudden joint changes post-menopause, hormone shifts are a prime suspect.”
How This Informs Real-World Care
Understanding this evidence changes the story—from “just aging” to “hormones matter here.”
Key insights for your toolbox:
- Hormonal shifts drive much of the joint pain seen at menopause, not simply years on the clock
- This means solutions can target both hormones and lifestyle—not just painkillers or blaming activity level
- If you’re wrestling with sudden, unexplained joint aches after menopause, you’re not imagining it—and there are research-backed reasons why
Picture this: Knowing that a drop in estrogen can spark a literal “joint storm” helps you (and your healthcare provider) pursue relief that fits the real biology, not just symptoms.
Bottom line? The best care for menopausal joint pain now targets its root cause—hormonal change is a key driver, supported by both science and real-world results.
Recognizing Menopausal Joint Pain: Symptoms and Common Patterns
Menopausal joint pain rarely sneaks up quietly—it’s often loud, persistent, and just a little bit unpredictable. If you’re in your 40s or 50s and suddenly stiffness, swelling, or “morning rust” have become part of your daily routine, you’re not alone.
Nearly 70% of midlife women report new or worsening joint symptoms around menopause. Picture this: waking up with aching knees, “creaky” hands, or a spine that feels two decades older—these scenarios are classic signals.
Common Symptoms: What to Look For
Most menopausal joint pain shows up as:
- Morning stiffness that lasts more than 30 minutes, but often eases with gentle movement
- Swelling in fingers, knees, or other joints—sometimes visibly puffy, sometimes just tender
- Diffuse aches—not just one joint, but several, moving around unpredictably
- Creaking or clicking sounds when you move, even if you’ve never noticed them before
- A deep, dull pain that flares after periods of inactivity or during weather changes
Where It Hits: Joints Most Affected
You’re most likely to notice discomfort in:
- Knees (“stairs suddenly seem steeper” moments)
- Hips (dull, hard-to-pinpoint aches)
- Hands (especially fingers—think trouble opening jars)
- Spine (a heavy, tired feeling after sitting)
“Menopausal joint pain doesn’t just target one spot—it roams.”
“If your body sounds like a bowl of Rice Krispies every morning, you’re in good company.”
Spotting the Difference: Menopausal vs. Other Joint Pains
How is menopausal joint pain different from just getting older or conditions like rheumatoid arthritis? Key clues:
- Menopausal arthralgia typically causes generalized aches and stiffness, often without major redness or heat
- Rheumatoid arthritis usually brings persistent, symmetrical swelling, plus possible heat and sudden joint deformity
- In most cases, imaging tests like X-rays are normal, even if pain is unmistakable
When to Get Checked: Red Flags
Don’t assume it’s “just menopause” if you notice:
- Joints that are red, hot, or severely swollen
- Rapidly worsening pain that doesn’t improve with medication or movement
- Unexplained weight loss, fever, or night sweats
- Persistent pain in one joint only
“If your symptoms shout ‘something’s not right,’ don’t tough it out—get evaluated by your provider.”
Menopausal joint pain is common, tricky, and linked to real biological changes—not just age. Spotting the classic patterns and red flags early means you can seek targeted relief and keep living life on your terms.
Laying the Groundwork for Relief: Strategies That Target the Root Causes
Understanding why menopause causes joint pain is your best launchpad for actual relief.
Instead of one-size-fits-all fixes, this knowledge lets you pick strategies anchored in the science: treat the cause, not just the symptoms.
Ask yourself: Is your pain showing up as morning stiffness, sharp twinges with movement, or an all-day background ache? Each clue points to a different root—and a matching relief strategy.
Tailoring Relief: Target the Underlying Mechanism
Root causes call for personalized game plans, including:
- Hormone therapy: Estrogen replacement can modestly reduce joint pain frequency, especially if started early postmenopause—backed by studies like the Women’s Health Initiative.
- Lifestyle shifts: Weight management, anti-inflammatory eating, and gentle activity help break the pain–inactivity–pain cycle.
- Physical therapy and strength work: Protects against cartilage degeneration, supports weaker joints, and restores muscle around problem areas.
- Non-hormonal options: NSAIDs, topical analgesics, or supplements like omega-3s and glucosamine target inflammation and pain from multiple angles.
Picture this: You add a daily walk, dial up your veggie intake, or trial topical anti-inflammatories—each small upgrade chips away at the whole pain puzzle.
Evolving Treatment: Adapting to the Latest Evidence
Treatment recommendations are always in motion as new studies roll out.
Right now, trends show:
- More women are combining hormonal and non-hormonal approaches for best results.
- Doctors increasingly recommend muscle-strengthening and flexibility routines, not just pain meds.
- Data show joint pain peaks early postmenopause—so timing matters when starting any intervention.
Remember: Addressing menopause joint pain isn’t just about “powering through.” It’s about smarter, more targeted action steps that fit your specific scenario.
Takeaway: Empowered Relief Starts Here
When you know what’s happening inside your body, you can choose relief options that work for your root causes—not just mask symptoms for a day.
Ready for details? The next step is exploring specific strategies—whether it’s hormone therapy, tailored exercise, smart self-care, or new medical options—each with their own practical roadmap for personalized relief.
Conclusion
Understanding the real connection between menopause and joint pain gives you the power to move beyond “just aging” explanations—and focus on what truly helps. When you recognize the role of hormones, lifestyle, and aging together, you unlock smarter, more strategic ways to protect your joints and reclaim your comfort.
Your toolkit for lasting relief starts with action, not guesswork. Here’s how you can begin to take charge today:
- Track your joint symptoms to spot connections with hormonal changes or lifestyle habits—and bring that data to your doctor.
- Move daily—even short, gentle walks or stretches count—because the right motion really is lotion for midlife joints.
- Consider proactive conversations about hormone therapy if menopausal symptoms are impacting your daily life (and ask for a tailored plan).
- Tweak everyday habits: add more anti-inflammatory foods, focus on maintaining a healthy weight, and break up long sedentary periods.
- Try non-hormonal solutions: topical NSAIDs, strength exercises, or supplements like omega-3s—for support from all angles.
You don’t have to navigate menopause joint pain alone or settle for band-aid solutions. Choose actions that fit your unique biology and lifestyle—and keep experimenting until you find what works best for you.
Need support? Reach out to a healthcare provider who understands women’s health in midlife, and don’t shy away from advocating for relief that addresses root causes.
Empowerment starts when knowledge meets action. Menopausal joint pain may be common, but with the right strategy, you can keep moving, keep strong, and keep control—one step at a time.
Your comfort is worth the effort—and you’ve got more options (and energy) ahead than you think. Share this insight, take the first step, and let better movement guide your next chapter.