Key Takeaways
Struggling with sleep during menopause? You’re not alone—and now, science-backed solutions go way beyond “just deal with it.” Here are the top research-driven strategies and practical actions for smarter, deeper rest—starting tonight.
- CBT-I is the gold standard for menopausal insomnia, with 60% of women reporting sleep issues and most seeing lasting improvements in just 4–8 weeks using digital, group, or telehealth options.
- Menopausal Hormone Therapy (MHT/HRT) sharply reduces hot flashes and night sweats, directly improving sleep—especially when micronized progesterone is taken at bedtime for a gentle, sedative effect.
- Tailor non-hormonal medications like SSRIs/SNRIs or gabapentin to your top symptom—these can cut nighttime hot flashes by up to 60% and help you wake up fewer times.
- Next-gen therapies like NK3R antagonists (fezolinetant) target the brain’s “internal thermostat,” showing a 50%+ reduction in hot flashes within 12 weeks and better sleep—perfect for those avoiding hormones.
- Revamp your sleep routine with high-impact tweaks: Keep a cool bedroom, set a regular sleep schedule, and limit screens and caffeine—with cooling strategies helping up to 85% of women sleep better.
- Screen for overlapping issues like sleep apnea or restless legs—nearly 50% of menopausal women with insomnia have another treatable sleep or health disorder boosting nighttime chaos.
- Partner proactively with your clinician using a 7-day sleep and symptom log and ask directly for top tools like CBT-I, hormone options, or screenings for stealth sleep problems—specifics lead to results.
Ready to turn restless nights into real rest? Dive into the full article for the exact how-tos and expert-backed shortcuts to reclaim energized, focused mornings at any age.
Introduction
You’re finally in bed after a hectic workday, but your brain won’t power down—and your body feels like it’s sabotaging your best efforts. Sound familiar? Nearly 60% of women in menopause experience sleep problems, and even tech-savvy professionals aren’t immune to these midnight disruptions.
Maybe you’ve tried the smart sleep trackers, tweaked your evening routine, or tested every cooling pillow Amazon suggested—only to be woken by a sudden hot flash or a restless mind running through tomorrow’s to-dos.
If you’re thinking, “How can I outsmart this?”—you’re in the right place.
Menopause doesn’t just hijack your hormones; it challenges your focus, creativity, and drive. For entrepreneurs, marketers, and innovators—those nights stolen by insomnia are more than an inconvenience; they’re productivity killers.
Here’s the good news: You have real, science-backed options to regain control.
Inside, you’ll discover eight actionable ways to transform your nights—ranging from tech-enabled therapy to precision medications, plus simple behavioral tweaks you can try tonight.
No fluffy “just relax” advice—each strategy is designed with busy, solution-oriented readers in mind, and includes:
- Clinically proven methods like CBT-I for insomnia
- Smart tech tools and telehealth options
- Hormonal and non-hormonal fixes for hot flashes
- Next-gen medications targeting your brain’s thermostat
- Lifestyle upgrades that fit your workflow—not fight it
True innovation happens when you merge cutting-edge science with practical, real-world application—and that includes your nightly routine.
You’re one article away from understanding the causes of menopause sleep disruption—and unlocking the latest solutions to feel sharper, more resilient, and in control.
So, what’s really disrupting your nights—and where’s the fastest path to better rest?
Let’s start by decoding the science behind those unpredictable sleep changes.
Why Menopause Disrupts Sleep: The Science Behind Nighttime Symptoms
When menopause hits, your sleep can become unpredictable—think tossing, turning, then staring at the clock at 3 a.m. wondering what changed.
The answer is in your hormones. As estrogen and progesterone levels drop, both brain and body chemistry shift in ways that directly impact sleep.
How Hormonal Shifts Trigger Nighttime Chaos
Menopause triggers a sudden change in sleep architecture for many women:
- Insomnia ramps up, with up to 60% of women reporting sleep problems during menopause.
- Night sweats can drench the sheets, causing abrupt awakenings.
- Frequent waking and early-morning arousal become the new norm for many, and just as you get comfy—bam—another hot flash hits.
“Imagine a thermostat that can't decide on a setting,” says Dr. Lisa, a menopause sleep specialist. Your body's internal temperature swings out of sync, thanks to hormone fluctuations, making deep, restorative sleep tough to hang onto.
The Toll of Vasomotor Symptoms and Sleep Disorders
Hot flashes and night sweats (aka vasomotor symptoms) do more than interrupt comfort—they literally fragment your sleep cycles:
- Core body temperature climbs, which cues your brain to wake up.
- These symptoms strike unpredictably, leading to broken sleep and groggy mornings.
Menopause also brings a greater risk for sleep disorders:
- Obstructive sleep apnea: Estrogen drop can relax airway muscles, so snoring becomes more common.
- Restless legs syndrome: Nighttime leg sensations ramp up in some women, making it nearly impossible to settle.
- Mood swings, anxiety, and depression: All three can spike during menopause—and each in turn steals away precious rest.
Why Restorative Sleep Is Essential—And Where to Start
Quality sleep isn’t just a luxury—it’s a menopause superpower. When you sleep well, you’re:
- Sharper at work and more creative,
- More resilient to stress,
- Better able to manage appetite, metabolism, and mood.
If sleep has become a struggle, start tracking your symptoms—like timing of night sweats or types of awakenings—so you can spot patterns and share evidence with your clinician.
Picture this: You wake up feeling refreshed, your mind clear, ready to tackle life and work. That’s the reality quality sleep during menopause can offer.
Prioritizing sleep isn’t just about feeling better—it’s a cornerstone for health, productivity, and day-to-day clarity as you move through menopause.
First-Line Solution: Harnessing CBT-I for Menopausal Insomnia
Cognitive Behavioral Therapy for Insomnia (CBT-I) stands out as the gold standard for tackling sleep problems during menopause—recommended by every major guideline for chronic insomnia.
If you’re wide awake at 3AM thanks to hot flashes or anxious thoughts, picture working with a sleep specialist who helps you design a playbook tailored for your real-life schedule, mood shifts, and nighttime wakeups.
What’s Inside the CBT-I Toolbox?
CBT-I isn’t just “sleep hygiene”—it’s a structured, science-backed approach made of:
- Sleep restriction: Temporarily limiting time in bed so you fall asleep faster
- Stimulus control: Training your brain to link the bedroom only with sleep or sex
- Cognitive reframing: Coaching you to unlearn unhelpful ideas like “If I don’t get 7 hours, my day is ruined!”
- Relaxation training: Teaching easy, on-demand ways to calm your body
- Sleep hygiene upgrades: Perfecting your environment and evening routine
“CBT-I is like a personal trainer for your brain at bedtime—focused, repeatable, and proven to change how you sleep.”
Why CBT-I Works for Menopause
Clinical studies show CBT-I sharply reduces insomnia severity, shortens the time it takes to fall asleep, and slashes nighttime awakenings—even for women juggling hot flashes and night sweats.
Meta-analyses found CBT-I works better than sleep medications or exercise alone for sleep problems tied to menopause.
- Women in digital or group CBT-I programs often see significant improvements in just 4–8 weeks
- After CBT-I, benefits last months—even years—without side effects or dependency
Imagine the relief of waking up refreshed, with fewer 2AM interruptions from intense heat or anxious tossing.
Accessing CBT-I: Modern Routes for Busy Lives
You don’t have to hunt down a sleep clinic in person.
CBT-I is available as:
- One-on-one or group sessions with a psychologist or sleep specialist
- Telehealth visits—get help without leaving your house
- Digital apps like Sleepio and Sleepstation, with user feedback showing real results (costs range from free trials to ~$30–$400/program; many clinics and insurers now provide access)
Tip: When talking to your doctor, ask specifically for “CBT-I”—not just “sleep hygiene tips.” Common advice like “cut caffeine” barely scratches the surface; you want the real, clinically proven program designed for insomnia.
The main takeaway: CBT-I is practical, customizable, and more effective than any quick-fix sleep aid. If restless nights are dragging you down, let a trained mind-body sleep strategy be your first move—science says it’s your best bet for real, restorative sleep during menopause.
When to Consider Hormone Therapy: MHT/HRT and Sleep Restoration
Why Hormone Therapy Might Be Your Next Best Step
If hot flashes and night sweats are sabotaging your nights, it’s worth exploring Menopausal Hormone Therapy (MHT/HRT).
When symptoms refuse to budge—despite solid sleep habits and CBT‑I—MHT/HRT may tip the balance toward restful sleep.
Picture this: you wake at 3 a.m., drenched and wide awake. MHT has been shown in a meta-analysis of 15,468 women to improve sleep quality while taming those disruptive flashes.
If you’re dreaming of a night without “temperature sprints,” you’re not alone.
What Hormone Options Actually Look Like
You’ll find systemic estrogen (think pills, patches, gels) at the heart of most MHT protocols.
- With a uterus? Add progesterone to protect your lining.
- Micronized progesterone, taken at bedtime, acts as a gentle sedative—making it easier to drift off and stay asleep.
- Triple win: better sleep quality, fewer awakenings, and lighter morning fog.
Social media snippet: “Night sweats and insomnia? Ask your doctor if bedtime progesterone could be your sleep superpower.”
The Evidence, Risks, and Real‑World Checklist
Evidence shows MHT not only reduces hot flashes but directly improves sleep disruption—especially when other methods haven’t delivered.
Still, MHT/HRT isn’t a one-size-fits-all answer. Here’s a practical checklist to tackle with your provider:
- Timing: Ideal if you’re peri- or newly postmenopausal (typically <10 years from your last period).
- Candidate review: Assess your personal risk—heart disease, breast cancer, migraines, blood clots.
- Formulation & delivery: Oral or transdermal estrogen? Bedtime progesterone?
- Current symptoms: Document how severe your sleep and vasomotor symptoms are—bring a brief journal.
Remember, most clinical guidelines now place CBT-I first, with MHT reserved for stubborn, severe symptoms that trash your rest.
Bringing It All Together
Consider hormone therapy when night sweats and hot flashes are relentless, especially if CBT‑I alone hasn’t restored your sleep.
By tracking symptoms and having a clear dialogue with your clinician, you can discover whether MHT or bedtime progesterone is the next step to reclaiming your nights.
Next-Level Support: Non-Hormonal Medications That Work
Trouble sleeping through menopause—even after trying lifestyle and behavioral tricks? Non-hormonal medications might be your next step for deeper, sweat-free nights. These aren't one-size-fits-all; the key is matching the right medication to your unique symptoms—whether it's hot flashes, anxious thoughts, or recurring insomnia.
Picture this: You're lying in bed, tossing, turning, heat swirling beneath your skin and frustration building. The right non-hormonal strategy could mean finally drifting off before midnight.
Targeting Vasomotor Triggers and Mood
If hot flashes and mood swings are sabotaging your sleep, several prescription options stand out. These have science on their side—helping over 50% of women reduce nighttime symptoms.
- SSRIs/SNRIs: (paroxetine, escitalopram, venlafaxine)
- Reduce hot flashes by up to 60% in clinical trials
- Improve mood and may indirectly boost sleep
- Start working within 1–2 weeks for many users
- Gabapentin: Especially helpful for sleep if night sweats are your nemesis
- Dual-action: lessens hot flashes and promotes drowsiness when taken at night
- Considered when SSRIs/SNRIs aren’t a match or hot flashes persist
These medications can be visually illustrated with a “before and after” scenario: waking drenched in sweat versus waking refreshed.
Sleep-Promoting Agents for Menopause
Struggling to fall or stay asleep—regardless of temperature? The newest sleep tools are designed for smoother nights and fewer side effects.
- Melatonin and prolonged-release melatonin
- Low-risk, over-the-counter support for sleep onset/maintenance issues
- Especially effective in women over 40 with mild insomnia
- Serotonergic and dual-action agents
- Newer medications combining serotonin rebalancing and sleep support
- Fitting for women needing ongoing, tailored assistance
- Dual Orexin Receptor Antagonists (DORAs):
- Think: “switching off” your wakefulness system
- Clinical promise for menopause-related insomnia, but consult your provider for fit and insurance coverage
All of these fit into a modern sleep toolkit that’s rapidly evolving.
Short-Term Sleep Aids: Last-Resort, Not Long-Term
Desperate for rest, but wary of “old-school” sleeping pills? Expert guidelines now strongly caution:
- Z-drugs (zolpidem, zaleplon) and benzodiazepines
- Short-term only—think days, not months
- Risks: Dependence, memory concerns, falls—especially post-menopause
- Use as a “bridge” while longer-term strategies (like CBT-I) take effect
A clear warning for anyone considering the quick-fix route: long-term use can backfire.
Here’s what to remember: Non-hormonal medications can dramatically cut hot flashes and help you reclaim your nights—especially when tailored to your specific symptoms. Come to your next clinician appointment with this list and ask which non-hormonal support fits best with your goals and health profile.
“Stop letting menopause call the shots—your best sleep could be one conversation away.”
“The right non-hormonal option bridges the gap between restless nights and brighter mornings.”
New and Emerging Therapies: The Cutting Edge of Menopausal Sleep Care
Welcome to the frontier of menopause treatment: Neurokinin-3 receptor antagonists (NK3RAs) are making headlines for their targeted approach to sleep disruption caused by hot flashes.
Unlike hormone-based options, these medications, such as fezolinetant, block specific brain signals that trigger hot flashes and night sweats—two of menopause’s top sleep wreckers.
Early clinical trials reveal:
- A 50%+ reduction in hot flashes within 12 weeks
- Noticeable improvements in both sleep quality and daytime energy
- Significant relief for women who can’t use, or prefer to avoid, systemic hormones
Picture this: You’re up at 3 a.m., sheets damp, wishing you could just reset your internal thermostat. Fezolinetant works directly on that internal thermostat, dialing down the heat waves that keep you awake at night.
Who Should Consider These New Options?
NK3RAs are well-suited for:
- Women who cannot take hormone therapy due to medical conditions or personal preference
- Those who’ve tried lifestyle tweaks, sleep hygiene, or non-hormonal meds and still struggle with nights fractured by hot flashes
- Anyone seeking a more precision-targeted treatment without the risks associated with estrogen-based therapies
What About Safety and Side Effects?
Current data shows:
- Most users experience few side effects—the most common are headache and mild liver enzyme changes (monitored with simple blood tests)
- No increased breast cancer or blood clot risk, setting NK3RAs apart from traditional hormone therapies
- Cost varies, with insurance coverage increasing as these drugs become more common
Best practice: Discuss potential risks, existing liver conditions, and medication interactions with your clinician. Regular bloodwork is typically recommended.
How Do These Fit Into a Personalized Sleep Strategy?
Think of NK3 antagonists as one more option in your toolkit, joining:
- CBT-I (proven behavioral therapy)
- MHT/HRT for those eligible
- Non-hormonal medications like SSRIs or gabapentin
- Lifestyle upgrades for cooling and relaxation
Your care team can mix and match these based on symptom severity, coexisting health factors, and personal priorities.
Summary: The emergence of NK3RAs like fezolinetant is a huge step for menopausal women who want targeted control over hot flashes and sleep—especially if hormones are off the table. Picture better sleep on your terms: the smartest way to unlock real rest in the menopause era.
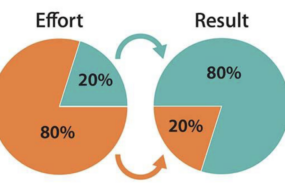
Proven Lifestyle, Sleep Hygiene, and Behavioral Upgrades
Getting menopause sleep right isn’t just about medication—tiny daily changes can transform your rest.
The most effective foundation? Sleep-supportive habits that set your brain and body up for deep, restorative nights.
- Stick to a regular schedule: Go to bed and wake up at the same times—even on weekends.
- Reserve your bed only for sleep and sex: No work, no Netflix marathons, no doomscrolling.
- Create a cool sleep sanctuary: Use cooling sheets, light bedding, and a quiet fan to combat night sweats.
“Picture this: it’s 3 a.m. and you’re sweat-soaked, tossing and turning. Now, imagine breathable sheets, a bedside fan, and your phone off—doesn’t that feel better already?”
Optimize Your Environment & Routine
Small tweaks have a big impact. In recent surveys, up to 85% of menopausal women reported improved rest with simple cooling strategies.
- Dim lights an hour before bed to cue your body’s natural sleep cycle.
- Keep electronics out of the bedroom (blue light from screens delays melatonin release).
- Limit caffeine after midday and cut back on evening alcohol—both worsen hot flashes and disrupt sleep quality.
A recent review found that late-night eating and vigorous exercise within 2–3 hours of bedtime reduce sleep quality for perimenopausal women. Try finishing dinner earlier and save workouts for morning or afternoon.
Wind Down and Sync Your Body Clock
Mind–body approaches are more than buzzwords—they work.
- Wind-down routines: A warm shower, gentle stretches, reading, or relaxation audios help signal sleep.
- Try progressive muscle relaxation, deep breathing, meditation, or gentle evening yoga—these ease the mind and lower anxiety.
- Daytime exercise and morning bright light exposure help synchronize your body clock (“circadian rhythm”) and make falling asleep easier at night.
Women who integrate these behaviors with medical or psychological treatments report less insomnia, fewer hot flashes, and greater energy the next day.
Want better sleep fast? Start with one bedroom tweak, one evening relaxation upgrade, and one caffeine cut—it’s a triple-win strategy you’ll actually feel in days.
Simple, science-backed shifts can deliver real results—especially when personalized to your menopause symptoms and layered with your clinician’s guidance. The right habits help medications and therapies work harder…putting restorative sleep back within reach tonight.
Addressing Overlapping Sleep and Health Issues
When menopause hits, sleep disruption often isn’t working alone—overlapping health problems are surprisingly common and often sneakily intertwined.
It’s not just about insomnia; in women over 40, rates of other sleep-disrupting conditions jump significantly.
Spot the Hidden Sleep Saboteurs
If sleep problems refuse to budge, consider these often-overlooked culprits:
- Sleep apnea (loud snoring, choking, morning headaches)
- Restless legs syndrome (RLS) (tingling or irresistible urge to move legs at night)
- Chronic pain (joint, muscle, fibromyalgia)
- Mood or anxiety disorders (persistent low mood, racing thoughts, irritability)
A 2022 analysis found that nearly 50% of menopausal women with insomnia have at least one overlapping condition.
Are You Due for a Sleep Check-in?
Don’t wait for symptoms to pile up. Watch for:
- Snoring, gasping, or high blood pressure (apnea warning signs)
- Leg discomfort or nighttime restlessness
- Ongoing pain that interrupts sleep or daily activities
- Persistent anxiety, depression, or mood swings
Picture this: It’s 2 AM, you’re awake again—not from hot flashes, but from aching legs or a pounding heart. These symptoms are not “just aging”; they’re red flags worth investigating.
Individualized, Layered Help Gets Results
Managing sleep and health in menopause is not one-size-fits-all.
The modern model combines:
- CBT-I for insomnia (either in person or digital)
- MHT or non-hormonal medication tailored to your underlying symptoms
- Targeted treatments for any co-existing issues (e.g., CPAP for sleep apnea, medication for RLS, pain management strategies, therapy for mood)
This layered approach is now standard in top clinics and sleep centers.
Ongoing Teamwork—Not a Solo Quest
No shame, no blame—these problems are common and highly treatable. Working with your care team means regular updates, tweaking strategies, and honest feedback.
One pro tip: keep a symptom and sleep log to track patterns and responses. This makes troubleshooting with your doctor faster and more precise.
If you take one thing from this, let it be this: Persistent sleep problems in menopause almost always have a treatable, sometimes hidden, cause. Addressing them head-on, with a personalized, layered plan, is the fastest way back to real rest.
Partnering With Your Clinician: Turning Knowledge Into Action
Picture this: You walk into your next appointment, equipped with specifics, not just symptoms—ready to transform your sleep game.
When it comes to menopause and sleep, the most effective outcomes happen when you actively partner with your clinician.
Bring a quick-reference sleep and symptom journal that tracks when you wake up, how often night sweats hit, and any mood shifts.
Your sleep journey is unique, and clinicians want data to personalize your roadmap.
What to Track and Bring
Prep your toolkit with these essentials:
- Sleep/wake times (including awakenings or restlessness)
- Note on hot flashes or night sweats and time of occurrence
- Mood changes, daytime sleepiness, or focus issues
- Any current medications/supplements and recent changes
A 7-day log is usually enough to spot patterns.
Essential Questions to Ask in Your Appointment
Here’s your powerhouse checklist for evidence-backed intervention:
- “Can you refer me to CBT-I—either a local therapist, group session, or a digital app like Sleepio?”
- “What are the pros and cons of MHT/HRT and is bedtime progesterone safe for me?”
- “Am I a candidate for non-hormonal options, like SSRIs/SNRIs, gabapentin, or melatonin?”
- “Should I be screened for sleep apnea, restless legs, or mood issues—and what tests are covered by my insurance?”
Leading with specifics lets your provider match you to the most effective, current strategies.
Keep the Momentum: Experiment, Record, and Feedback
After your visit, think like a sleep detective.
Try one change at a time: adjust light exposure, swap to cooling sheets, or shift exercise to morning.
Record impacts in your journal.
Don’t wait for yearly checkups: update your clinician with email check-ins or app logs—most platforms now support remote tracking and feedback.
Memorable Takeaways for Action
- “If you don’t log your symptoms, you’re flying blind—track for clarity, not just curiosity.”
- “Partnering means asking for gold-standard tools, not just accepting ‘sleep hygiene’ as a fix.”
- “Your path to restful sleep is built in bite-sized breakthroughs, not overnight overhauls.”
A collaborative approach turns scattered sleep complaints into a structured, actionable plan—one you can actually stick with. Take charge, track everything worth tracking, and never settle for half-hearted solutions.
Conclusion
Real, rejuvenating sleep during menopause is possible—especially when you blend science-backed strategies with a clear, proactive plan. By tuning into your body’s needs and leveraging the latest tools, you can outsmart those 3 a.m. wakeups and reclaim the rest you deserve.
Every step you take—whether it’s tracking symptoms, fine-tuning your environment, or collaborating with your clinician—brings you closer to deeper, more restorative sleep. The key is choosing solutions that fit your unique rhythm and making small, consistent changes that add up fast.
- Streamline your sleep journal: Log wake times, hot flash patterns, and mood shifts for one week to uncover actionable insights.
- Ask for gold‑standard treatments: Request a referral for CBT-I or access a reputable digital program—don’t settle for generic advice.
- Upgrade your bedroom: Focus on cooling strategies—breathable bedding, a bedside fan, and light pajamas can change your nights.
- Stay open to new therapies: If symptoms persist, discuss emerging options like NK3RAs or tailored non-hormonal meds with your provider.
- Sync up with your doctor: Share your tracked data and ask targeted questions to create your personalized sleep playbook.
Start today: Choose the one change that feels most doable—order cooling sheets, download a CBT-I app, or book a deeper conversation with your clinician. Momentum builds with each choice you make.
Sleep disruption doesn’t have to define your menopause journey. When you get strategic, experiment bravely, and partner with the right experts, better nights—and bolder, brighter days—are entirely within reach.
Own your rest, rewrite your story, and show menopause who’s in charge of your sleep from tonight onward.