Key Takeaways
Ready to revolutionize your approach to diabetes management? Here’s what every tech-savvy professional should know about how exercise reshapes diabetes outcomes in 2026. Scan these actionable tips to unlock the science, strategies, and real-world hacks that put better control right at your fingertips.
- Exercise is now a first-line treatment for both type 1 and type 2 diabetes, rivaling medication for impact on blood sugar control and overall health.
- Just one workout boosts insulin sensitivity and improves glucose uptake for up to 72 hours, helping you make every session count.
- Consistent aerobic activity lowers HbA1c by 0.5–0.7 points, while resistance training can improve insulin sensitivity by 48%—combine both for the strongest results.
- Personalized activity targets are data-driven in 2026: adults should aim for 150–300 minutes/week of moderate-to-vigorous aerobic exercise plus resistance training 2–3 times weekly for optimal outcomes.
- Breaking up sitting time is essential—active breaks every 30–60 minutes (like short walks or stretches) can quickly lower average blood sugars and boost energy.
- Timing and intensity matter: Afternoon workouts yield better glucose drops and higher medication-free rates, while HIIT delivers results fast for busy schedules.
- Smart tech and wearables transform adherence—AI coaching boosts workout consistency by 38% and cuts HbA1c by 0.5 points over 8 months, with CGMs giving instant, actionable feedback.
- Education and motivation are crucial: Structured programs, real-time data, community support, and gamification drives long-term habit change—turning movement into your most effective diabetes tool.
Staying active isn’t just an add-on in 2026—it’s your most versatile, tech-empowered prescription. Want the full strategy to transform your diabetes outcomes? Dive into the main article for the how and the why behind every step.
Introduction
Take a moment to picture this: a single gym session can boost your insulin sensitivity for up to 72 hours—and that’s not just headline hype, it’s the reality for people living with diabetes in 2026.
If you’re juggling tech, business, and glucose stats (or helping others do the same), you know that “move more” advice usually feels vague and outdated. But latest science—and some serious shifts in medical guidelines—have turned exercise into a smart, personalized power tool for anyone managing blood sugar.
What’s changed? Exercise is no longer the sidekick to meds or gadgets—it’s now a front-line therapy as critical as your prescription or your favorite CGM. Today’s strategies go way beyond “just walk more”:
- Ultra-targeted activity plans tailored by age, job, and schedule
- Breakout research on timing and intensity—think “afternoon surge” or micro-bursts at your standing desk
- Seamless integration with AI-driven wearables, making every step, stretch, or ride measurable (and far more motivating)
You’ll get answers to questions like:
- How do aerobic, resistance, and HIIT workouts actually rank for HbA1c and TIR?
- What’s the smartest way to stack movement throughout a jam-packed workday—without sacrificing results?
- How do new ADA guidelines help you minimize the risk of hypoglycemia (and wasted effort)?
- Which digital tools, social strategies, and evidence-backed hacks stick for real people?
No matter your technical know-how or fitness background, you’ll see how a bit of smart movement can transform daily management—sometimes even reducing medication. Expect practical frameworks, credible stats, and actionable next steps, not motivational fluff.
Curious how a single tweak in your routine could flip your diabetes care from exhausting to empowering?
You’re about to see why movement in 2026 is the new must-have—more customizable, science-backed, and efficient than ever.
So, how exactly does physical activity outperform tradition and technology for diabetes outcomes?
Let’s pull back the curtain on the latest science and start with what makes movement such a potent tool.
The Science of Exercise in Diabetes: Why Movement Is a Game-Changer
Looking for a single upgrade to supercharge your diabetes management? Exercise might be the closest thing to a “universal remote” for blood sugar.
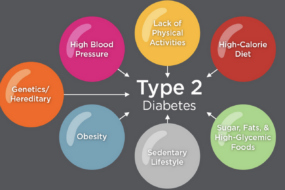
In both type 1 and type 2 diabetes, physical activity acts as an “on switch” for glucose metabolism—literally moving sugar out of your bloodstream and into hungry muscles.
Recent research confirms: Just one session of aerobic or resistance exercise can improve insulin sensitivity and boost glucose uptake for up to 72 hours. That means your body uses insulin more efficiently, making the most of every workout.
Exercise and Glycemic Control
Numbers speak volumes—here’s what the latest guidelines and studies show:
- In type 2 diabetes, aerobic exercise regularly lowers HbA1c by about 0.5–0.7 percentage points
- Resistance training alone reduces HbA1c by ~0.57 points and can ramp up insulin sensitivity by roughly 48%
- Combining aerobic and resistance (“concurrent”) training delivers the biggest bang for your buck: Best-in-class HbA1c drops, more time-in-range (TIR), and wider cardiometabolic benefits
- For type 1 diabetes, days with structured activity boost TIR and 24-hour mean glucose but require smart tactics to prevent hypoglycemia
Picture this: Every brisk walk or gym session nudges your glucose stats into healthier territory—sometimes lowering the need for medication altogether.
The Ripple Effects: Cardiometabolic and General Health Benefits
Exercise delivers far more than better glucose numbers.
Here’s what regular movement has been shown to achieve in people living with diabetes:
- Lower blood pressure
- Improved lipid profiles (think: better cholesterol)
- Sustainable weight management
- Noticeably increased cardiorespiratory fitness
- Decreased risk for heart attack and stroke
But it’s bigger than metrics—people often report higher energy, less stress, and sharper focus after making movement a habit. One walk can change your numbers; a routine can change your life.
Daily choices to get moving—whether that’s cycling, stair-climbing, or dancing in your kitchen—create positive ripples that extend to every corner of diabetes care. If you want a smarter, more powerful way to dial up your diabetes control, consistent exercise is your most versatile tool.
2026 Guidelines: The New Rules for Physical Activity in Diabetes
Staying active is no longer a suggestion—it's a front-line treatment for diabetes in 2026. The American Diabetes Association (ADA) and global health leaders now define physical activity as essential as medication for managing both type 1 and type 2 diabetes.
Today's guidelines push for more movement for everyone and far less sitting.
Personalized, Data-Backed Activity Targets
Forget one-size-fits-all. The ADA’s 2026 update brings crystal-clear “doses” tailored to your life phase:
- Youth (children/teens):
- Get at least 60 minutes daily of moderate-to-vigorous activity
- Include bone and muscle strengthening exercises several times per week
- Adults:
- Aim for 150–300 minutes per week of moderate-to-vigorous aerobic activity
- Add resistance training 2–3 days every week for maximum benefit
- Popular ways people hit these targets:
- Brisk walking, cycling outdoors or on a smart trainer, group sports, HIIT classes, weekend hikes, and even “microbursts” like climbing stairs or active play
- Everyday movement counts too—think walking meetings, grocery lugging, or parking farther away
These numbers aren’t random—they reflect the sweet spot where statistics show HbA1c drops by 0.5–0.7 points and many adults need fewer diabetes medications after one year.
“Movement is your most underrated prescription—now it’s fully individualized, science-backed, and flexible enough to fit any calendar.
The New Focus: Breaking Up Sitting Time
The old advice was to “exercise most days.” The 2026 approach? Never let sitting win for too long.
Long workday at a desk? Don’t wait for the gym—insert quick, energizing movement every hour.
- Try standing desks or treadmill workstations
- Take 2–5 minute activity breaks every 30–60 minutes: short walks, squats, or stretching
- Swap one video call per day for a brisk “walk and talk”
Just these tweaks can drop average blood sugars within days—and keep energy up, not just numbers in range.
“Imagine your workspace as a launchpad: a few steps, a stretch, or a set of stairs are now considered as valuable as your next Zoom invite.”
Real-World Support for Busy Lives
Everyone’s routines are different, so leading recommendations have dropped rigid rules:
- You’re no longer “failing” if you break exercise into short bursts
- All physical movement—at home, at work, in transit—counts toward the total
- Flexible routines are proven to increase confidence and adherence over time
“In 2026, the best exercise plan is the one you’ll actually do—workouts, errands, laughter, unexpected dance breaks all included.
Whatever your schedule or fitness level, minimizing sedentary time and moving often are now non-negotiable for diabetes management. This is the new era where exercise is as essential as any prescription—and finally fits real life.
Exercise Modalities: Matching Fitness Routines to Diabetes Outcomes
Aerobic Exercise: Endurance for Glycemic Stability
Aerobic activities—like walking, running, cycling, and swimming—stand out for their impressive track record in blood sugar management.
For people with type 2 diabetes, regular aerobic exercise typically lowers HbA1c by 0.5–0.7 percentage points. Think of this as earning an extra 30–45 minutes of daily time-in-range (TIR) just by making movement a habit.
What's happening under the hood? Insulin sensitivity and glucose uptake surge for 24–72 hours after a single aerobic session—meaning each workout pays dividends for days. Picture a brisk morning walk turning into measurable glucose improvements at your next checkup.
Resistance Training: Building Muscle, Boosting Insulin Action
If you prefer strength and definition, resistance training delivers. Here’s what’s often recommended:
- Frequency: 2–3 days/week, hitting all major muscle groups
- Approaches: Machines, free weights, bands, or even bodyweight exercises
Studies report an average HbA1c drop of about 0.57 points, and some trials show a 48% boost in insulin sensitivity—that’s more efficient glucose handling without extra medication.
Want to see a visible difference? Imagine improved muscle tone and metabolic health translating into less reliance on medication.
Concurrent and HIIT Approaches: Maximizing Benefits
Here's the secret sauce for many: pairing aerobic with resistance—or dabbling in HIIT (high-intensity interval training).
- Concurrent training: Yields the largest HbA1c reductions and best overall health outcomes
- HIIT: Matches moderate steady-state exercise for glycemic benefits, while also improving VO₂peak and reducing insulin resistance
But a quick word for planners—HIIT’s intensity might require customized tweaks for safety, especially if you’re adjusting meds or worried about hypoglycemia. Think “power walks with short sprints” or full-body circuits—short, impactful, and backed by robust data.
Customizing Your Fitness Formula
Different modalities deliver unique benefits, but the best approach ties to your personal style and goals. Are you energized by brisk walks, gym routines, or fast-paced group classes?
Swapping sitting for even brief movement unlocks measurable health wins.
Try this: build your week around variety, and notice how smarter movement makes life with diabetes more predictable—and a little more fun!
Key insight: “Every movement counts, and the right combination is tailor-made for you.” This is exercise personalization, 2026-style.
Timing, Intensity & Personalization: Making Exercise Work for You
Dialing in the when, how hard, and how personal you make your workouts can majorly ramp up results—and lower your risk—whether you’re managing type 1 or type 2 diabetes.
The right timing or intensity tweak can mean the difference between steady glucose or a surprise swing, better energy, and, yes, even dropping a medication.
Chronotype and Activity Timing
When you exercise isn’t just about what’s convenient—it matters for blood sugar and medication outcomes.
- Afternoon workouts led to the greatest 1-year glucose drop and a higher chance of stopping diabetes meds, according to the Look AHEAD study of over 2,400 adults.
- People most active in the afternoon saw faster improvements than morning or random-timers.
- Morning sessions may benefit early risers or those wanting stable pre-work glucose, but you’ll want to test what works for you.
Picture this: It’s 4pm, you hit the park for a brisk walk, and you’re stacking the odds for medication-free living.
Quotable: “Afternoon activity = more time in range, fewer pills, and a shot at more freedom.”
Intensity Matters: Moderate, Vigorous, and HIIT
Not all workouts are created equal—intensity shapes your body’s response and your time investment.
- Moderate intensity = brisk walk, heart up but you can chat; best for steady results.
- Vigorous = jogging, cycling hard, music up, hard to talk; more rapid gains, but prep for higher glucose swings.
- HIIT (High-Intensity Interval Training) = short, powerful bursts; matches moderate exercise for glucose benefit when total effort equals out.
Latest studies show:
- HIIT and steady workouts both lower HbA1c in type 2 diabetes (about 0.5–0.7 point reduction).
- For time-crunched pros, HIIT means results—in less time.
Quotable: “Short on hours? HIIT packs a week’s work into minutes—just hit those intervals hard.”
Personalization Strategies for Different Diabetes Types
No two bodies—or routines—are the same, so match your tactics to your profile.
- Type 1: Focus on glucose checks before/after, and adjust carbs or insulin, especially with vigorous or longer sessions.
- Type 2: Consistency over perfection—goal is 150–300 minutes/week, but mixing up types and times keeps it achievable.
- Consider:
- Age and fitness history: Start gentle, progress as confidence builds.
- Comorbidities: Joint issues? Go for cycling or pool, not pounding runs.
- Culture and preferences: Love group Zumba, or prefer solo hikes? Both work—embrace what motivates you.
Quotable: “The best exercise is the one you’ll actually do—and keep doing.”
Fine-tuning the timing, intensity, and personal touches of your workouts not only keeps diabetes in check, but also helps you find a rhythm you’ll stick with. The right combo can unlock better blood sugars, fewer meds, and real-world results you’ll feel every day.
Navigating Risks and Barriers: Safety, Education & Motivation
Facing exercise with diabetes in 2026 means not just knowing what to do, but how to stay safe, motivated, and confident each step of the way.
One major challenge, especially for folks with type 1 diabetes? The fear of hypoglycemia. In fact, it’s the #1 reason many hesitate to jump into new routines or sports.
Managing Hypoglycemia and Glucose Swings
How your blood sugar reacts to movement depends on the type of workout:
- Aerobic exercise (like jogging) can drop glucose the fastest—often within 30–60 minutes.
- Interval and HIIT workouts offer a gentler swing, with less sudden dips.
- Resistance training (think weights) typically causes the smallest glucose drop and may even bump levels up at first.
What does this mean for real life? Protocols make all the difference:
- Always check blood sugar before starting.
- If low (<100 mg/dL), have 15–30g of fast-acting carbs handy—think glucose tablets or juice.
- Adjust insulin before/after: talk to your care team about reducing rapid insulin or pump rates around activity.
Even with automated insulin delivery, expect a slight increase in time below range on exercise days. Pre-exercise prep is truly your secret weapon.
These adjustments don’t just help athletes—they’re a lifeline for anyone ready to chase better health and “normal” days.
“One smart tweak in your workout routine can slash hypoglycemia worries and make every session safer.”
Leveraging Education & Technology
Knowledge is (blood sugar) power—especially in 2026:
- Structured exercise education for newly diagnosed youth boosted TIR by an extra 3.1% (~45 minutes/day) after just a few sessions.
- Wearables and CGMs now give real-time alerts, helping you spot dips early and adjust on the go.
- Diabetes apps and smart devices build confidence, letting you see your body’s response in vivid data.
Picture this: You lace up, check your app, and get instant feedback on workout timing, fueling, and insulin tweaks—making every session more predictable and, honestly, empowering.
Keeping It Real: Motivation and Adherence Hacks
Let’s bust the “I hate exercise” myth—movement can actually be fun and stick long-term:
- Gamify your step counts or workouts using leaderboards and challenges.
- Set mini, doable goals (“Two walks this week before work”) instead of aiming for perfection.
- Recruit an accountability partner or support squad—your family or your team at work.
Don’t underestimate the power of a cheering section or swapping a standard meeting for a walk-and-talk. These little shifts turn “have to” into “want to.”
Remember: Small changes in routine can unlock big gains in health, energy, and confidence. For every potential barrier, there’s a smart workaround ready, whether it’s tech, teamwork, or simply reframing what movement means for you.
The Future of Diabetes Fitness: Innovation, Research & Practical Trends to Watch
The way you move with diabetes in 2026 is about smarter tech, smarter routines, and smarter support. If you haven’t met your digital “fit-friend” yet, get ready—virtual trainers and AI-powered routines are here, making your workouts more personalized and proactive than ever.
Integrating Digital Health & Wearables
Picture this: Your smartwatch and continuous glucose monitor (CGM) are in constant conversation.
- CGMs and fitness wearables now sync in real time, instantly translating your activity into actionable advice
- Algorithms adjust your goals, send alerts for target heart rate or glucose thresholds, and even suggest snack breaks
In recent digital coaching pilots:
- Adults using AI-driven coaching reported “workout adherence went up by 38%,” and HbA1c dropped an average 0.5 percentage points over 8 months
- In-app reminders and friendly nudges have made skipping sessions a thing of the past
That’s not just motivation—that’s precision support 24/7.
Ongoing Research and Emerging Best Practices
Researchers are testing everything from mini “exercise snacks” (as short as 4 minutes!) to immersive home-based programs that gamify movement.
Key studies for 2026 highlight:
- Group routines delivered through virtual platforms boosting engagement by up to 51%
- Structured “exercise prescriptions” that tailor timing and type of exercise based on your glucose curves and daily schedules
Imagine seeing your workout plan adjust the moment your morning CGM trend spikes, or receiving safe, evidence-based tips for intervals when busy workdays keep you sedentary.
Shaping a More Active Future: Community and Advocacy
No one achieves lasting change alone. Forward-thinking employers, schools, and clinics are building “movement-friendly” environments where motion is built in—not something you have to squeeze in.
You’ll see:
- Standing meetings and lunchtime walking clubs at work
- After-school fitness squads and gym class upgrades for kids
- Peer-led activity groups and telehealth accountability circles for all ages
Today’s advocacy focuses on smashing barriers—physical, digital, and psychological.
For anyone with diabetes, access isn’t optional—it’s a right. “If everyone can move, everyone can improve.”
The future of diabetes fitness puts real-time data, supportive communities, and adaptive routines squarely in your corner. Picture a world where every movement makes a measurable difference—starting now.
Conclusion
The future of diabetes management is active, personalized, and undeniably empowering. Your daily movement isn’t just another box to check—it’s your most potent tool to take control, reduce medications, and unlock better energy and health.
Advances in science and technology mean you can now leverage exercise for results that fit your lifestyle, not the other way around. It’s less about perfection and more about progress—one step, one session, one smart tweak at a time.
Here’s what you can put into practice now:
- Swap long stretches of sitting for mini movement breaks—even a two-minute walk or stretch impacts your blood sugar
- Mix up routines with aerobic, resistance, and HIIT sessions for the biggest payoff in glucose control and motivation
- Leverage wearable tech or digital apps to personalize your schedule, get real-time feedback, and catch highs or lows before they’re a problem
- Make movement social—schedule a “walk-and-talk” meeting or invite a peer for accountability
- Don’t wait for perfect conditions—every bit of activity, from chores to meetings, counts toward your diabetes goals
Ready to jump in? Pick one small change that fits your week—book a standing meeting, set a wearable reminder, or try an afternoon walk tomorrow. Track the difference and let your results drive tomorrow’s motivation.
You hold the remote—push play on movement, and watch not just your numbers, but your confidence and quality of life, transform.
Every decision to move today shapes your health, your independence, and your future. This is how you revolutionize your diabetes story, starting right now.