Key Takeaways
Managing diabetes means more than just watching your blood sugar—it’s about seeing your mouth and body as a fully connected system. If you want fewer dental surprises and smoother glucose control, these practical, research-backed strategies will give you an immediate edge. Here’s what you can put into action right now:
- Blood sugar control is your oral health foundation—tight glucose management can reduce your risk of gum disease, slow wound healing, and mouth infections by up to 50%.
- Oral problems and diabetes have a two-way impact—even mild gum disease can raise A1c by 0.3-0.4%, making glycemic control tougher.
- Professional dental care is non-negotiable—visit your dentist every 3–6 months for periodontal screenings, oral cancer checks, and early intervention that keeps treatments simple and cost-effective.
- Perfect your daily routine for major payoffs—brushing twice daily (preferably with an electric toothbrush), daily flossing, and choosing fluoride rinses or gels can cut dental emergencies and expenses.
- Watch for red flags and act quickly—don’t ignore swollen gums, persistent bad breath, or slow-healing sores, since early action prevents bigger complications and blood sugar spikes.
- Teamwork between your dentist and diabetes provider is a game-changer—sharing your latest blood sugar numbers and medication changes can cut post-procedure infection rates by up to 50%.
- Tackle dry mouth head-on—sip water often, use xylitol gum, and skip alcohol-based rinses to lower your cavity risk and boost comfort throughout the day.
- Smart lifestyle changes deliver double wins—prioritize fiber-rich foods, quit smoking, and get active to both stabilize blood sugar and strengthen your gums, leading to 40% fewer dental emergencies.
Put these insights to work, and you’ll build a diabetes-friendly oral care game plan that protects both your smile and your overall health. For step-by-step strategies and tech-savvy tips, check out the full guide!
Introduction
Ever noticed your mouth feeling drier than usual, or that your gums bleed after a quick brush—even though you’re pretty diligent about your oral care? You’re not alone. More than 60% of people with diabetes battle gum disease, and many have no idea it’s quietly sabotaging both their smile and their blood sugar.
What if you could spot trouble early, keep toothaches from wrecking your workday, and actually shave numbers off your A1c—all by upgrading your mouth-care routine? Oral health isn’t just a dental issue for those with diabetes—your teeth and gums are on the frontlines of your overall health.
Here’s where things get interesting for anyone who values efficiency: mouth problems don’t just tag along for the diabetes ride—they amplify it. Inflamed gums and mouth infections can push your blood sugar higher, turning tiny annoyances into stubborn health setbacks.
The upside? You can build a smarter, AI-inspired self-care workflow for your mouth—no PhD required. In the next few minutes, you’ll discover:
- How diabetes and gum health create a feedback loop—and break the cycle before it starts
- The action steps that work in the real world: from daily dental habits to smoother, tech-friendly provider communication
- Signals your mouth is sending right now (and the simple tweaks that prevent routine checkups from becoming emergencies)
Whether you’re optimizing routines as a business owner or building next-level workflows as an AI enthusiast, understanding the mouth-body connection multiplies your wins. Better oral care isn’t just about avoiding a trip to the dentist—it’s a power move for your diabetes and your long-term health.
Ready for a new perspective? Let’s explore how your mouth could be the most overlooked—and most fixable—predictor of your diabetes control.
You might never look at your toothbrush the same way again.
Understanding the Link Between Diabetes and Oral Health
Diabetes and oral health have a powerful, two-way connection. High blood sugar can harm your mouth, and, in turn, mouth problems can make managing diabetes much tougher.
Picture this: your mouth acts as the frontline in your diabetes battle—it’s where hidden issues can stir up the biggest trouble before you ever spot them.
Why People With Diabetes Are at Higher Risk
When blood sugar levels are elevated, the landscape of your mouth changes dramatically. You’re not just at higher risk for cavities—your defenses against bacteria and infection take a serious hit.
You’re especially prone to:
- Gum disease (periodontitis and gingivitis)
- Persistent dry mouth (xerostomia)
- Frequent mouth infections (bacterial or fungal, like thrush)
- Sores or wounds that are slow to heal
Even a short stretch of out-of-range glucose can trigger sore, swollen, or bleeding gums—sometimes before you even feel sick.
How High Blood Sugar Changes Your Mouth
With diabetes, think of sugar as fuel for bacteria. Elevated glucose levels in saliva provide a feast for harmful germs, leading to inflammation and weak tissue repair.
- Infections are harder to fight off due to a less responsive immune system.
- Healing after dental work or injury takes longer—sometimes weeks, not days.
- Saliva thickens or decreases, cranking up discomfort and cavity risk.
Quotable: “Think of your teeth and gums as the early alert system for your overall health.”
The Two-Way Street: Mouth Problems and Blood Sugar Control
Oral issues don’t just stay put—they can push blood sugar levels even higher. There’s a cycle:
- Developing gum disease can spike A1c by 0.3-0.4% on average.
- Mouth pain and infection can stress your body, potentially raising glucose.
Notice persistent bad breath, soreness, or new mouth problems? They're not just dental annoyances—they may signal a deeper glycemic struggle.
Oral Health Awareness Surges in 2026
By 2026, awareness is rising: more people (and their providers) are making the mouth-body link a part of their regular care. Still, over 60% of people with diabetes experience some form of gum disease—and most don’t realize it’s making glucose harder to control.
Small changes, like seeing your mouth as a health barometer, can give you a proactive edge. If your gums feel like the weak link in your diabetes armor, it’s time to team up with your dentist and take action before small problems spark bigger ones.
Key takeaway: Regular oral care and blood sugar management are inseparable—protecting your mouth pays dividends for your entire diabetes journey.
Foundation First: Blood Sugar Control and Oral Health
Keeping your blood sugar in check is the absolute foundation for great oral health—think of it as the cornerstone on which every other strategy rests.
Tight glycemic control doesn’t just protect your heart and nerves; it directly lowers your risk for gum disease, cavities, infections, and those dreaded slow-healing mouth sores.
Think about this: People with well-managed diabetes face significantly less gum disease than those with frequent highs and lows—a fact backed up by years of research.
The Domino Effect: What Happens When Blood Sugar Runs High
When blood sugar spikes, it sets off a chain reaction:
- More inflammation in your gums, making them puffy, red, and prone to bleeding
- A weaker immune system, so mouth bacteria have a field day
- Trickier healing after dental treatments or even small injuries
Ever noticed your gums getting especially sore or puffy after a string of elevated blood sugars? You’re not imagining things—this is the diabetes/oral health loop in action.
Two-Way Street: Gum Health Also Impacts Diabetes
Here’s a powerful stat: Treating gum disease (like with deep cleanings or periodontal therapy) can lower your HbA1c by up to 0.4%—a modest but meaningful boost for your diabetes game.
Uncontrolled oral infections can also make it tougher to control your blood sugar. Your body cranks out stress hormones during infections, often sending glucose levels even higher.
Real-World Hurdles and Action Steps
Managing your mouth with diabetes means dealing with extra curveballs, like:
- Oral infections making blood sugar stubbornly unpredictable
- Needing more frequent check-ins with both your dentist and doctor
- Navigating wound healing that takes just a bit longer than you’d like
The good news: Every single step toward lower average sugars—whether that’s improving your meal timing, moving more, or keeping up with meds—has a real impact on your smile.
For anyone living with diabetes, remember this: “Your mouth is both a reflection and a regulator of your overall diabetes control.”
Taking charge of your blood sugars won’t just make your doctor happy—it can quite literally save your gums, teeth, and that confident grin. It’s a win for your mouth, your body, and your peace of mind.
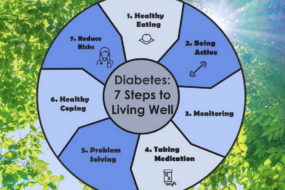
Building Your Oral Care Routine: Step-by-Step Strategies
Daily Habits for a Healthier Mouth
Think of your daily oral care as non-negotiable armor in the diabetes battle—done right, it dramatically slashes your risk of infections and dental bills.
Here’s what needs to be on your checklist:
- Brush twice each day with fluoride toothpaste—morning and night.
- Consider an electric toothbrush; it removes plaque nearly 21% better than manual for many users.
- Clean between your teeth once daily—use floss, interdental brushes, or a water flosser. Pick whatever’s actually easy for you to stick with.
- Go for a fluoride rinse or gel at bedtime if your dentist says you’re high risk (think more than two cavities in the past year).
- If your mouth gets dry, choose non-alcohol-based mouthwash—alcohol will only make dryness worse. Antimicrobial rinses also knock down bacteria.
Picture this: The difference between casually scrubbing and a focused routine is like “throwing your clothes in a pile versus actually folding them and putting them away.”
Special Moves for Problem Areas
Not all mouths have it easy—sensitive gums and dexterity issues call for smart tweaks.
If you see bleeding or soreness:
- Switch to a soft-bristled brush and gentle pressure
- Use flexible flossers or water flossers to clean without pain
If you have arthritis, neuropathy, or shaky hands, try these strategies:
- Use an electric toothbrush with a thick handle (easier to grip)
- Go for floss picks or pre-threaded flossers over regular string
Work with your dentist if your mouth is in rough shape. Many can create home care plans tailored for “problem spots” or difficult teeth.
Nighttime Dental Care & Reminders
Night is prime time for damage if you let oral care slide, especially when high blood sugar means more bacteria hanging around.
To protect yourself:
- Set a reminder to brush/floss every evening—timers, sticky notes, or a phone alert all work.
- Apply fluoride gels or prescription pastes right before bed if you’ve been told you’re high risk.
- Keep water bedside for midnight dry-mouth relief.
A few daily tweaks save you hours in the dentist’s chair and potentially hundreds on complex procedures.
Small, consistent habits pay major dividends—mastering your oral routine is one of the most cost-effective ways to prevent diabetes complications.
Dentist Visits and Periodontal Care: What to Expect
Frequency and Types of Dental Care Needed
If you have diabetes, you’ll want to see your dentist every 3–6 months—and sometimes more often if your gums are giving you grief.
Routine exams aren’t just for finding cavities. You’ll get:
- Full periodontal checks to catch gum disease early
- X-rays to spot hidden problems below the surface
- Oral cancer screenings, especially important if you have longstanding diabetes
Picture this: catching mild gum inflammation means less pain (and expense) down the road. Early intervention often prevents bigger complications—and helps keep your blood sugars smoother, too.
“Checking in with your dentist is like running a regular system scan—address small issues before they crash your workflow.”
Working as a Team With Your Dentist
Great dental care for diabetes isn’t just about what your dentist does—it’s a real collaboration.
At each visit, be ready to:
- Share your diabetes status, including recent blood sugar numbers
- Bring a list of all your current medications, since some interact with dental treatments or affect healing
- Discuss any new symptoms—bleeding gums, dry mouth, slow healing sores
Dentists who know your diabetes details can:
- Adjust appointment timing to your glucose rhythms
- Tailor wound care to your healing speed
- Plan infection prevention steps proactively
“Think of your dentist as your oral health project manager—together, you’ll make smarter, faster decisions.”
What Happens During and After Appointments
Before your visit, eat as usual and take your regular diabetes meds unless your provider says otherwise.
Pack these essentials:
- Your updated medication list
- A note of your most recent blood sugar or A1c values
- Fast-acting glucose tabs or snacks, just in case
If you have extractions or deep cleanings coming up, expect:
- Slightly longer healing times if your glucose is running high
- The need to watch for red flags: swelling, fever, or wounds that aren’t closing up
- Calling your dentist promptly if something feels off—don’t tough it out
A single dental appointment can feel like hitting ‘refresh’ on your whole oral health routine.
It all comes down to connection: Regular dental visits, honest communication, and smart preparation turn your dentist into a key ally in your diabetes care. Building this partnership helps you avoid bigger oral (and blood sugar) problems later—so you can focus on what matters most.
Red Flags: Warning Signs You Shouldn’t Ignore
Your mouth often sends out early warning signs when something’s off—especially if you’re managing diabetes.
Don’t brush aside small annoyances; in diabetes care, a tiny gum issue today can snowball fast.
If you spot any of these symptoms, it’s time to book a dental visit:
- Red, swollen, sensitive, or bleeding gums
- Persistent bad breath or a strange, metallic taste that won’t quit
- Loose teeth or your bite suddenly feels “off” (teeth shift, eating feels weird)
- Unrelenting dry or burning mouth
- Trouble swallowing or chewing
- White patches (possible fungal infection like thrush)
- Sores that heal slowly or keep coming back
Why Quick Action Beats Waiting
Delaying care lets problems escalate—think of gum disease like a spark in dry grass.
Left alone, a simple irritation can turn into a full-blown infection or even tooth loss.
Research shows people with diabetes face twice the risk for severe gum issues—and infections can push your blood sugar upward for days or even weeks.
If you’re tracking oral symptoms alongside your glucose log, you’ll spot trends early and help your dentist and doctor team up on smarter care.
How to Track and Share Symptoms
Keeping a running list of changes—date, severity, and how long they last—makes it way easier for your provider to spot patterns.
Try noting:
- How often you’re dealing with bad breath or bleeding gums
- Whether dental pain flares up after a series of high blood sugars
- Any mouth changes that coincide with new medications
Pro tip: “Don’t wait for a local fire to become a full-blown inferno—get help at the first spark.”
What Happens When You Act Fast
Treating small problems early almost always means:
- Less discomfort (and anxiety) for you
- Easier, less expensive solutions
- Better blood sugar stability—a double win
Addressing red flags early is your smartest move. A quick call at the first twinge could save you weeks of pain, costly procedures, and a major disruption to your diabetes management.
Dry Mouth Solutions: Staying Comfortable and Cavity-Free
Understanding Dry Mouth in Diabetes
If you’re managing diabetes and feel like your mouth is stuck in “desert mode,” you’re not alone.
Dry mouth—also called xerostomia—is a frequent side effect of both high blood sugar levels and some common diabetes medications, like metformin.
When saliva slows to a trickle, you might notice:
- Sticky or dry sensation
- Trouble chewing, swallowing, or even speaking
- An increased risk of mouth sores and cavities (because saliva naturally helps protect your teeth)
- That “burning mouth” feeling, especially at night
A 2024 study found up to 60% of people with diabetes report symptoms of dry mouth at least weekly.
Tools and Tips for Relief
The good news? A handful of simple strategies can make your mouth feel less like the Sahara—often starting today.
Start with these hydration habits:
- Sip water frequently throughout the day (keep a bottle at your desk or by the sofa)
- Avoid soda, sports drinks, or juice—sugary beverages actually worsen dryness and ramp up cavity risk
- Skip caffeine and alcohol, both notorious mouth-dryers
Try these saliva-saving tools:
- Xylitol gum or lozenges—stimulate saliva, taste sweet, won’t spike blood sugar, and can cut cavity risk
- Safe-for-diabetics saliva substitutes or mouth moisturizers (available over the counter)
- Humidify your workspace or bedroom if the air feels dry, especially overnight
For food and drink choices:
- Choose soft foods (think yogurt, stews, smoothies) if chewing is challenging
- Limit salty snacks and spicy foods—they tend to make dryness worse
- Absolutely avoid tobacco and alcohol-based mouthwashes, as both intensify dry mouth
If your symptoms stick around or keep you uncomfortable despite these tweaks, it's worth:
- Asking your provider if a medication change is possible
- Requesting a dental prescription for a high-fluoride toothpaste or gel to add extra cavity defense
Picture this: stepping into a meeting, your mouth feels refreshed, not parched—even after a full morning on Zoom.
Subtle, daily moves like choosing water over soda or popping a xylitol mint can add up fast for comfort. Dry mouth isn’t just annoying—it’s a real risk for your teeth, so proactive care pays off. The right routine keeps your smile safer, your conversations easier, and your day a lot more comfortable.
Lifestyle Moves That Support Both Oral and General Health
Diet and Nutrition for Mouth and Metabolism
Let’s start with the kitchen: your food choices shape both your blood sugar and your gum health, often in a single bite.
Picture this—you’re prepping lunch, reaching for fiber-rich vegetables, lean protein, and whole grains. These picks keep your glucose stable and nurture healthy gums.
For anyone with diabetes, a low-added-sugar diet isn’t just about A1c—it’s about cavity prevention, too. Sugary snacks fuel oral bacteria, leading to gum inflammation and tooth decay.
It’s not just what you eat, but when and how often. To maximize mouth health:
- Space out meals and stick to set snack times (less grazing = fewer bacterial acid attacks)
- Include vitamin C and D-rich foods (think oranges and salmon) to speed gum healing
- Incorporate omega‑3s (flaxseed, walnuts, tuna) for their proven anti-inflammatory impact
- Sip water throughout the day—dry mouth and cavities skyrocket when you get dehydrated
A simple swap, like moving from soda to water or herbal tea, makes a tangible impact in just a week.
“Every meal is a double investment—fuel for your metabolism and protection for your smile.”
The Big Picture: Smoking, Sleep, Exercise, and Stress
Let’s talk habits. Some pack an unexpected punch—like smoking, which multiplies your risk for severe gum disease and delayed healing if you've got diabetes.
Looking for an oral-health upgrade? These “stacked habits” make a difference:
- Quit smoking—it’s the fastest way to halt “silent” gum loss and stubborn infections
- Prioritize sleep (aim for 7-8 hours nightly): poor sleep impairs your mouth’s immune defenses
- Schedule movement breaks or daily exercise to reduce chronic inflammation and aid healing
- Practice quick stress resets (deep breathing, five-minute walks) to regulate blood sugar and reduce flare-ups
Today, a single habit shift can shave dollars off your future dental bills and make checkups less stressful—research shows active patients spend 40% less on emergency dental treatments.
“Think of exercise as floss for your metabolism—and your gums.”
Balancing your meals, quitting smoking, and getting enough sleep form the base of a resilient, diabetes-friendly oral care routine. Small steps now stack up to bigger health (and fewer dentist visits) all year long.
Coordinating Care: Bridging the Gap Between Dentist and Diabetes Team
Clear communication between your dentist and diabetes care team isn’t just a nice-to-have—it’s vital for preventing complications.
When it comes to living with diabetes, your mouth and your metabolism are more connected than most people realize.
Sharing up-to-date info between providers helps every appointment work smarter for you, not harder.
When Extra Coordination Is Critical
Some situations demand top-tier teamwork:
- Major dental work, like extractions or implants
- Poorly controlled blood sugar (A1c above 8.0%)
- Medication changes (especially starting steroids, new diabetes meds, or immunosuppressants)
- A history of delayed healing or frequent oral infections
Imagine you’re scheduled for gum surgery and your doctor just adjusted your insulin—your dentist needs those details before planning the procedure.
How Better Collaboration Changes Outcomes
It’s not just talk: studies show that coordinated care can shorten healing times, cut infection rates by up to 50%, and reduce overall treatment costs.
When dentists and doctors share:
- Glycemic status (recent A1c, daily blood sugars)
- Medication lists (diabetes drugs, blood thinners, immunosuppressants)
- Surgical plans and special wound-care needs
…they tailor your care to prevent surprises and speed up recovery.
One real-world example: A patient with uncontrolled diabetes had preventive antibiotics and a custom wound-care routine before wisdom tooth removal—healed in half the usual time and avoided infection.
Proactive Communication: What You Can Do
You’re the info super-connector:
- Bring medication lists and latest blood sugar readings to all dental and medical visits
- Tell both teams about upcoming procedures or medication shifts
- Ask questions when something doesn’t add up; don’t just nod along
A quick update can make a huge difference: “Small details shared early can prevent big problems down the road.”
Trending Forward: Team-Based Care in 2026
Healthcare in 2026 is trending toward digital health portals, shared records, and virtual case conferences between your providers.
Leaders are piloting AI-powered alerts that ping your dentist and doctor simultaneously if records show a new medication or a lab trend.
Picture this: You’re prepping for a deep cleaning—an app notifies both your dentist and endocrinologist, prompting a team check-in and real-time care adjustment.
The key takeaway? You drive faster healing and less stress by making sure your care teams talk to each other. Your mouth—and your blood sugar—will thank you for it.
Navigating Dental Appointments With Diabetes
Picture this: It’s the morning of your dental appointment, and you’re determined not to let diabetes throw a wrench into things. With the right prep, you’ll sidestep blood sugar drama and keep healing on track—a little planning goes a long way.
Your Pre-Appointment Safety Checklist
Getting ready isn’t just about showing up—there’s a lot you can do to make your visit smooth and stress-free:
- Eat as you normally would to keep your blood sugar steady
- Take your usual diabetes medications unless told otherwise by your provider
- Check your blood sugar at home before you leave (and log your recent values for easy reference)
- Pack quick glucose snacks (like juice boxes or glucose tablets) in case you dip low in the chair
- Bring an up-to-date list of all medications and supplements
Three minutes of prep can spare you hours of frustration—so don’t skip it.
Food, Meds, and Blood Sugar at the Dentist
Dental appointments rarely fit neatly into your day. Here’s how to stay a step ahead:
- Tell the staff you have diabetes, and share your current blood sugar
- If your reading is below 100 mg/dL, consider a snack before you’re called back
- For longer or invasive procedures, ask about scheduling during the morning (when you’re most stable)
- Monitor your blood sugar after the appointment, especially if you had anesthesia or skipped a meal
Dental anxiety can nudge blood sugar up, so acknowledging your stress helps everyone keep you safer.
Handling Highs, Lows, and Emergencies
Even with planning, surprises can happen—so be ready:
- If you feel shaky, dizzy, or sweaty, let the dentist know immediately
- If your blood sugar runs higher than 250 mg/dL at check-in, postpone nonessential procedures and review your diabetes plan
- Always mention recent infections, changes in medications, or hospitalizations
One quotable reminder: “Bringing snacks to the dentist is a life hack, not an overreaction.”
Post-Procedure Do’s and Don’ts
Healing starts the moment you leave the chair. Here’s your low-stress care plan:
- Follow all wound care instructions—don’t take shortcuts
- Keep eating and taking diabetes meds as usual unless your dentist says otherwise
- Call your provider if you notice redness, swelling, pain, or a fever that isn’t subsiding
- Watch for signs of infection—sore spots, oozing, or slow healing aren’t normal
If something feels off, quick action saves bigger problems—and bigger bills—later.
Feeling proactive at the dentist means showing up with your blood sugar plan, asking direct questions, and giving your future self a pat on the back for staying in control. Being prepared at every step is how you transform dental visits from stressful events to confident, manageable routines.
Conclusion
Empowering your oral health isn’t just about a brighter smile—it’s a direct investment in making diabetes management easier and more predictable. Prioritizing small, consistent habits with your mouth gives you more control, more energy, and a buffer against complications that can affect every part of your life.
You’ve seen that the strongest diabetes strategy is one where your dentist, doctor, and daily routine work together—because when your gums are healthy, your entire body gets a boost.
Key takeaways to put into play right now:
- Treat daily oral care as an essential part of your diabetes routine—brush, floss, and rinse with intention.
- Track early warning signs (like bleeding gums or dry mouth) and act quickly to cut off bigger problems.
- Sync up dentist and diabetes appointments—share health updates between providers for coordinated, smarter care.
- Stay hydrated and cut back on sugary foods and drinks, since both your blood sugar and your mouth will thank you.
- Reach out for tailored guidance—if you notice anything new, don’t wait to consult your care team.
Ready to take action? Here’s how to move forward:
- Schedule your next dental checkup and set a reminder on your phone.
- Review your oral care tools—pick up an electric toothbrush, flossers, or dry mouth aids as needed.
- Update your medication list and keep it handy for all appointments.
- Share one new oral health goal with your care team or accountability partner today.
When you make your mouth a priority, you’re taking command of your diabetes journey—smarter, stronger, and more confidently than ever.
Think of it as your daily upgrade: every small step adds up, and your future self will thank you for protecting your healthiest smile (and body!) today.
“Your healthiest days start with the habits you build now—your mouth is the smartest place to begin.”